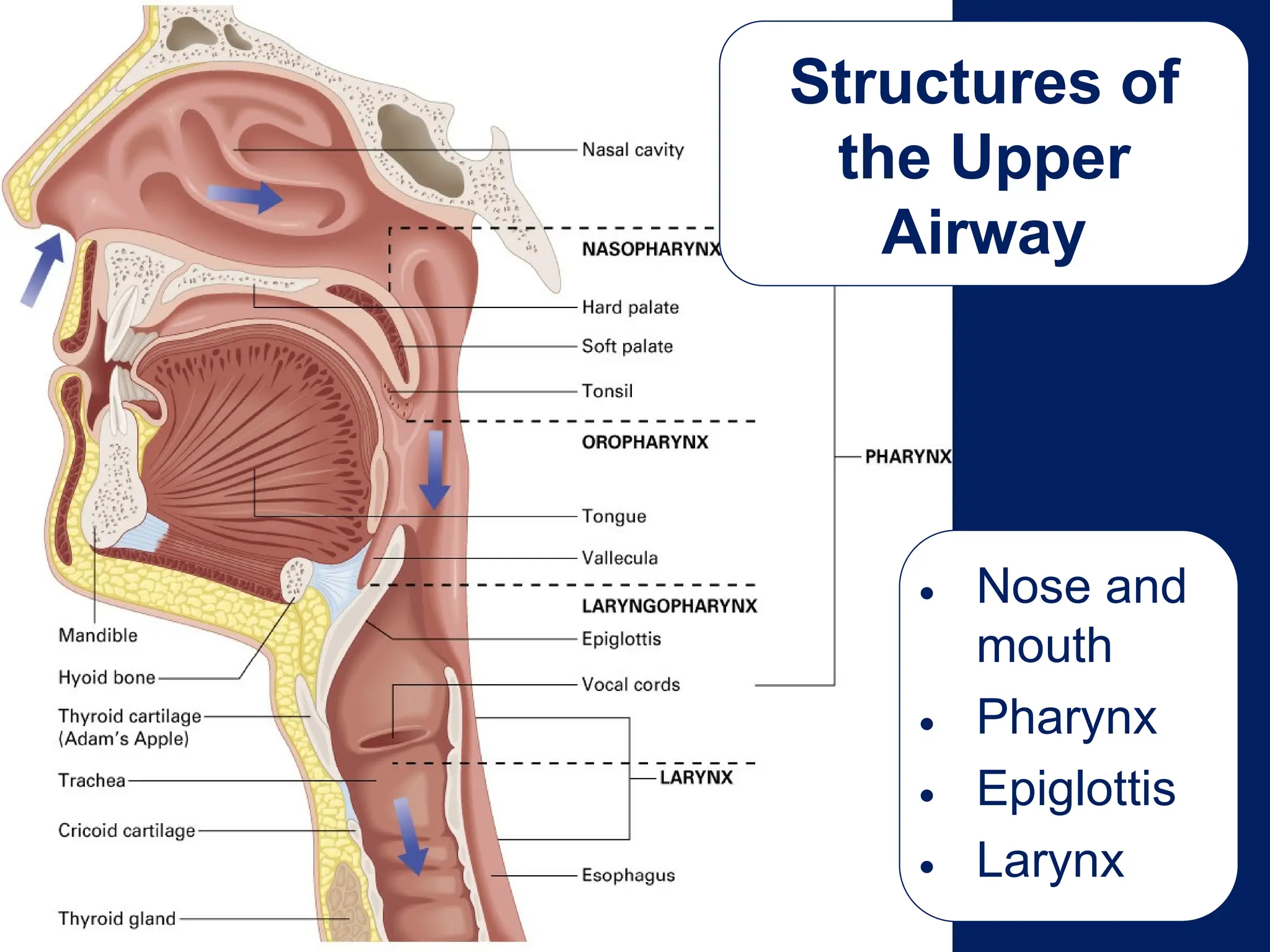
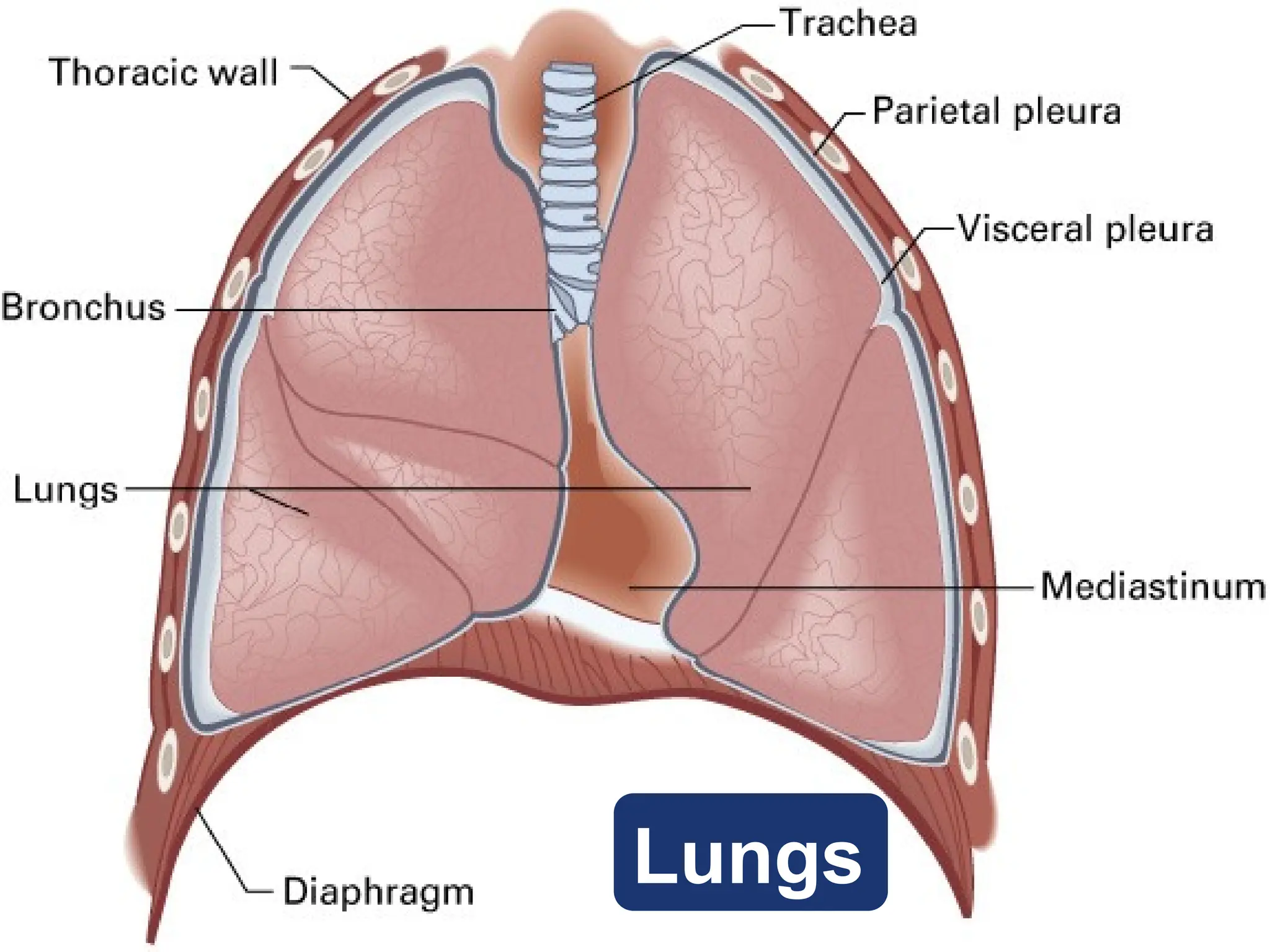
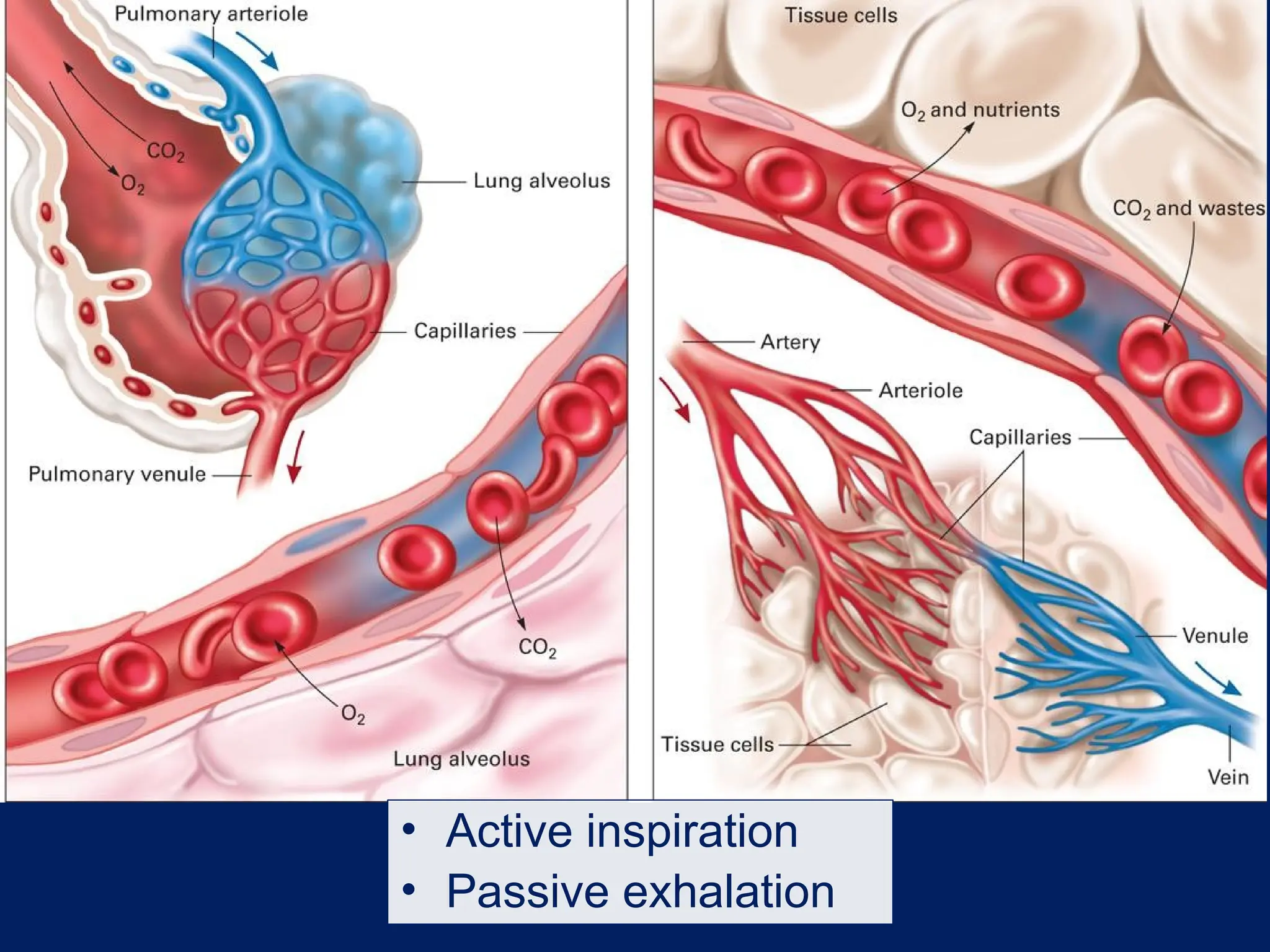
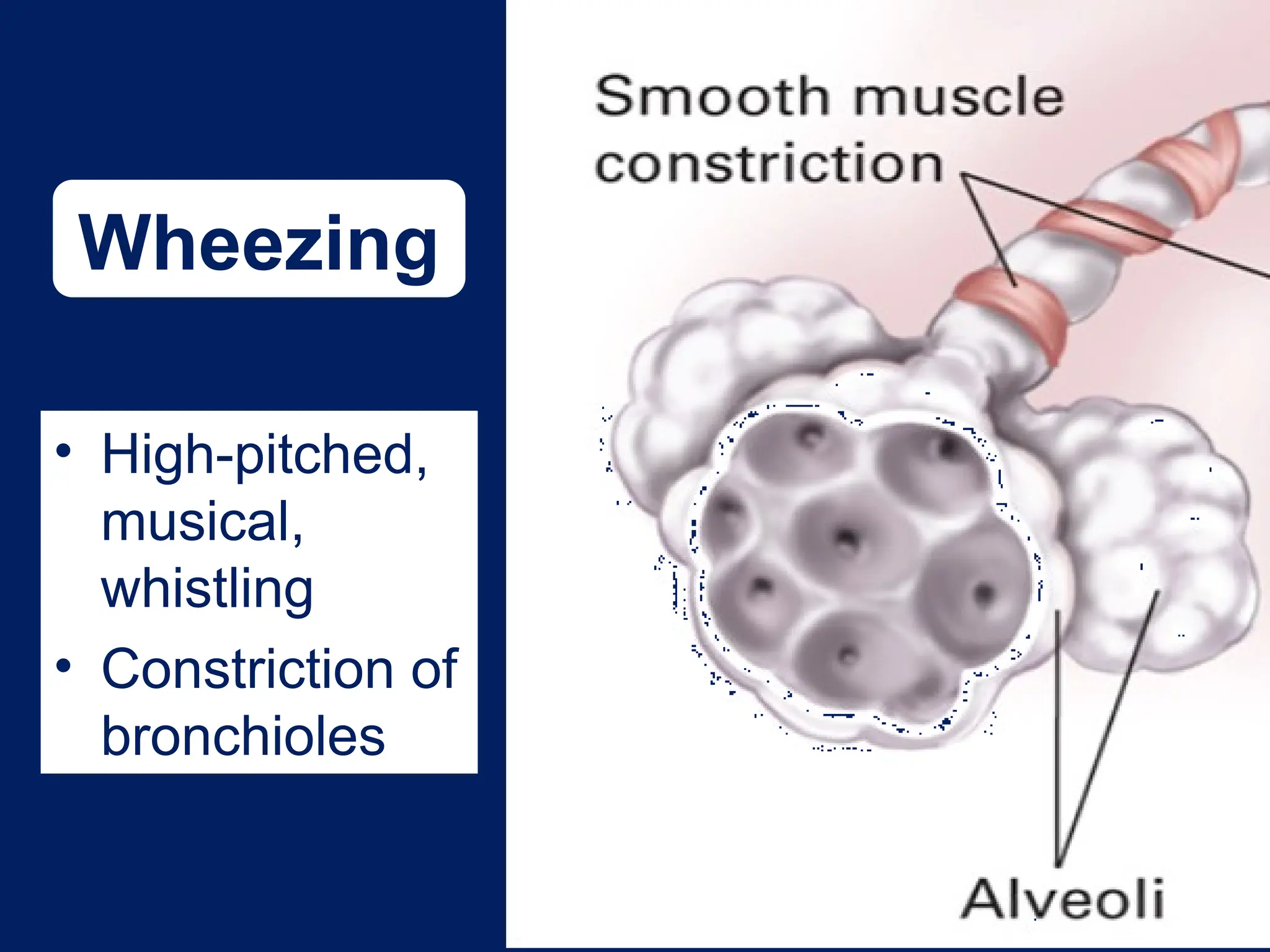
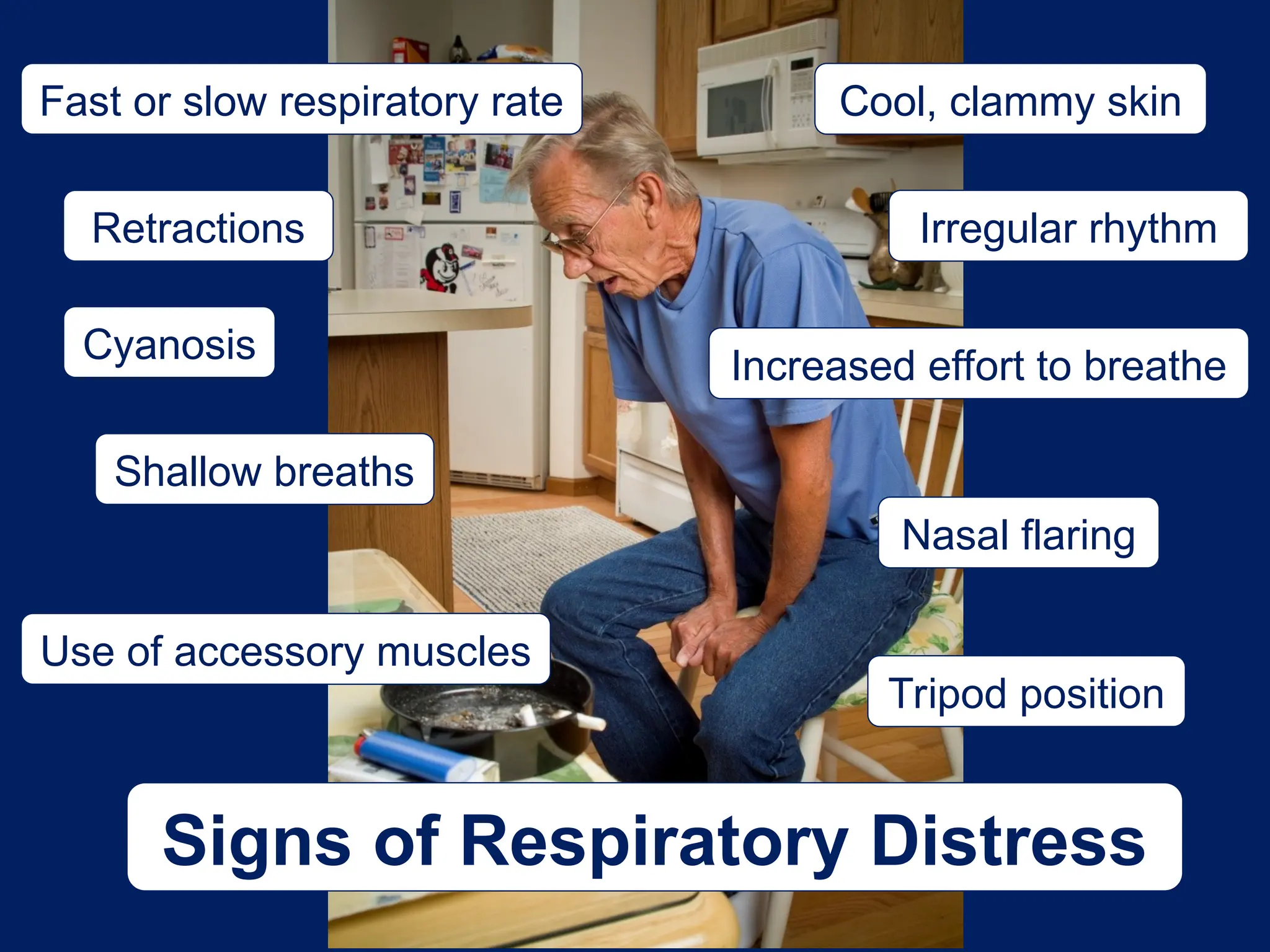
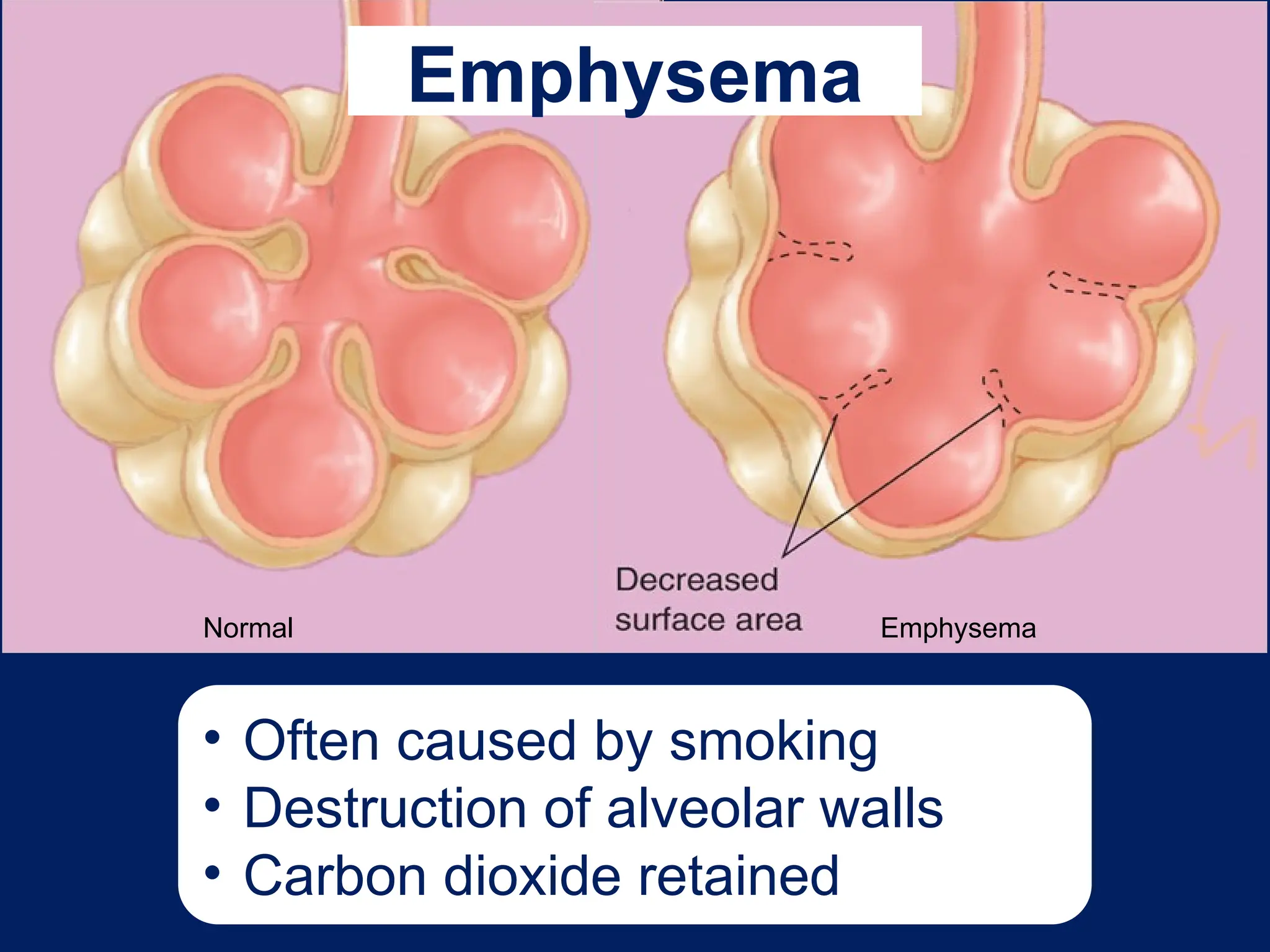
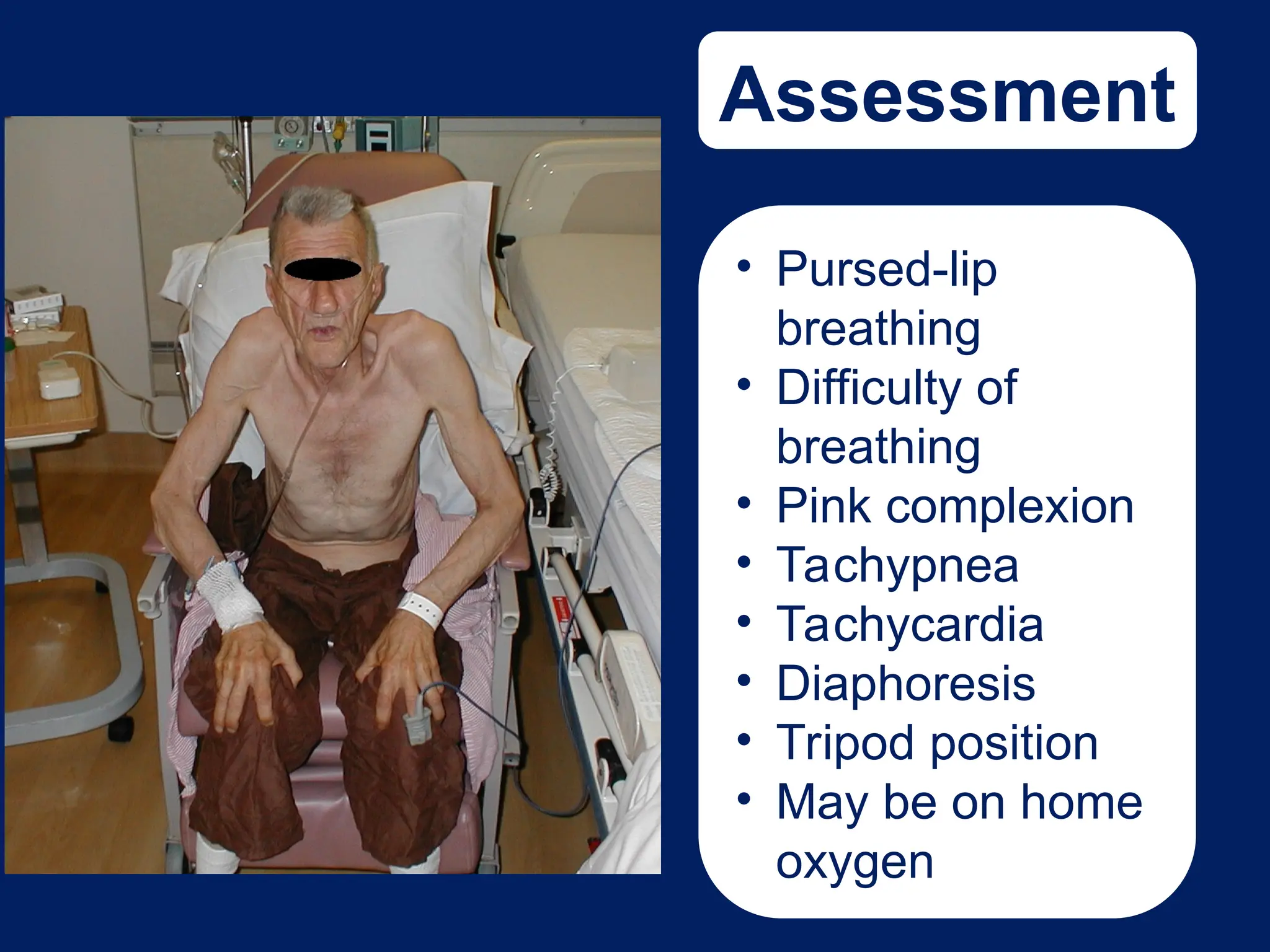
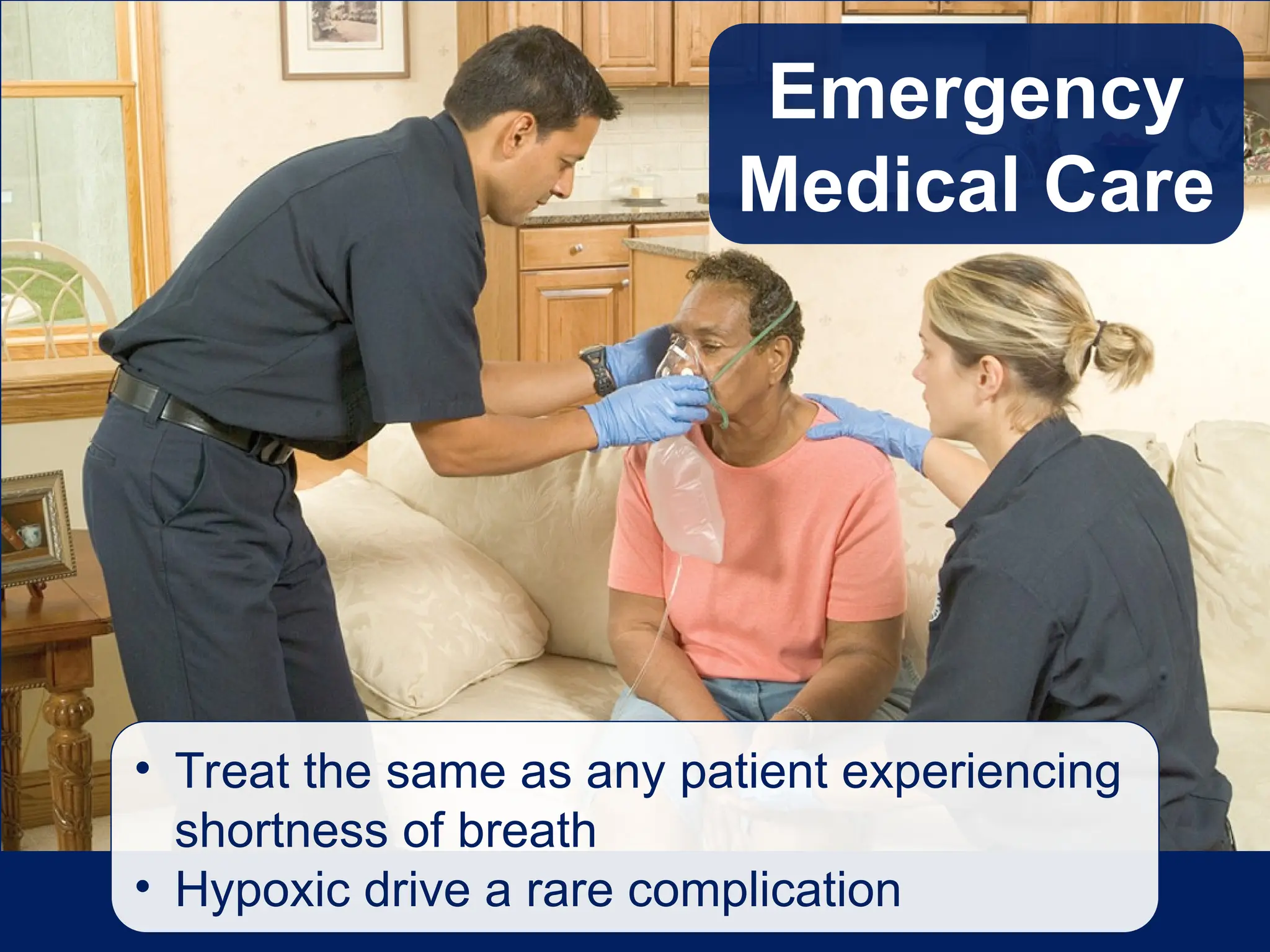
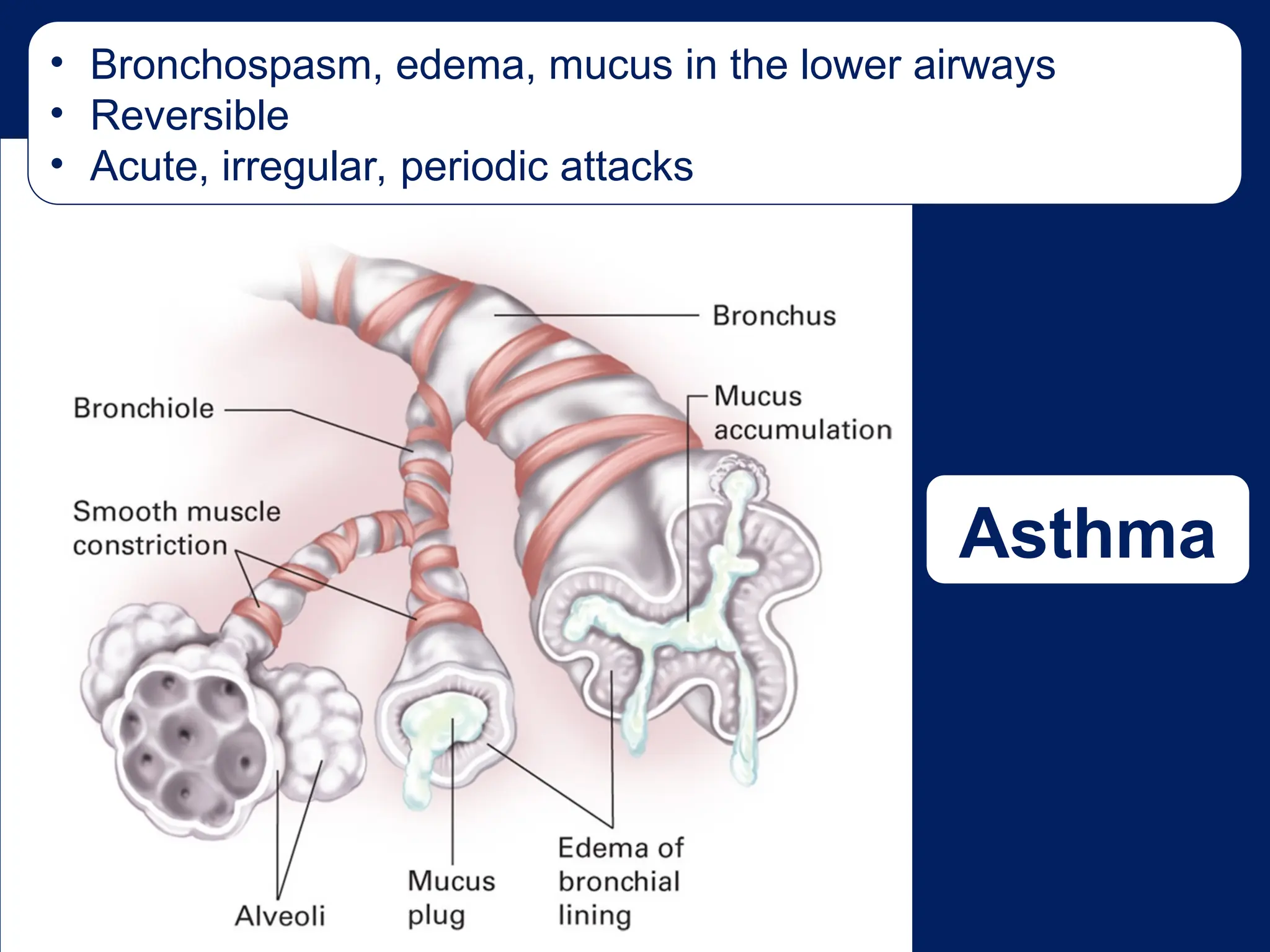
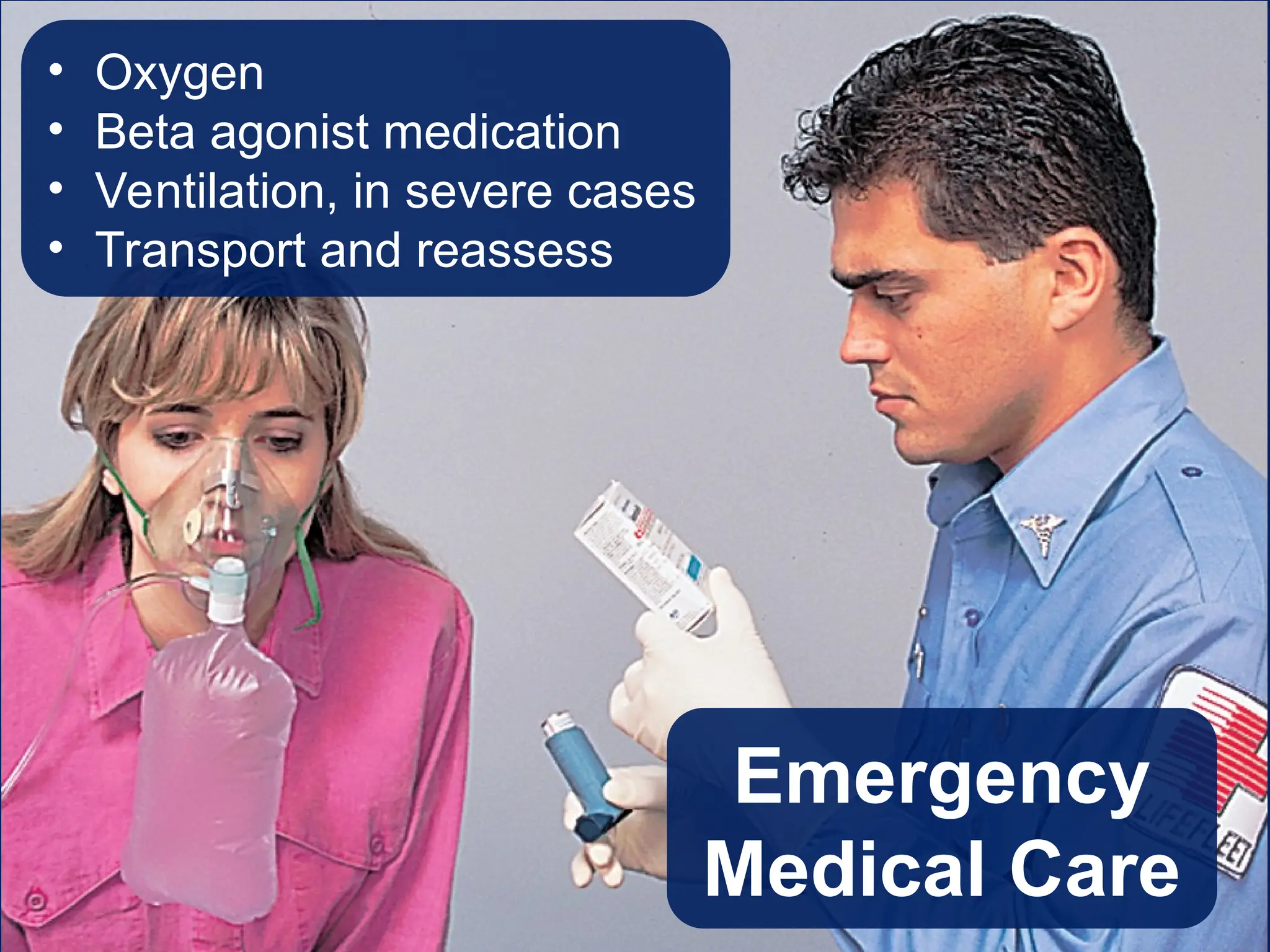
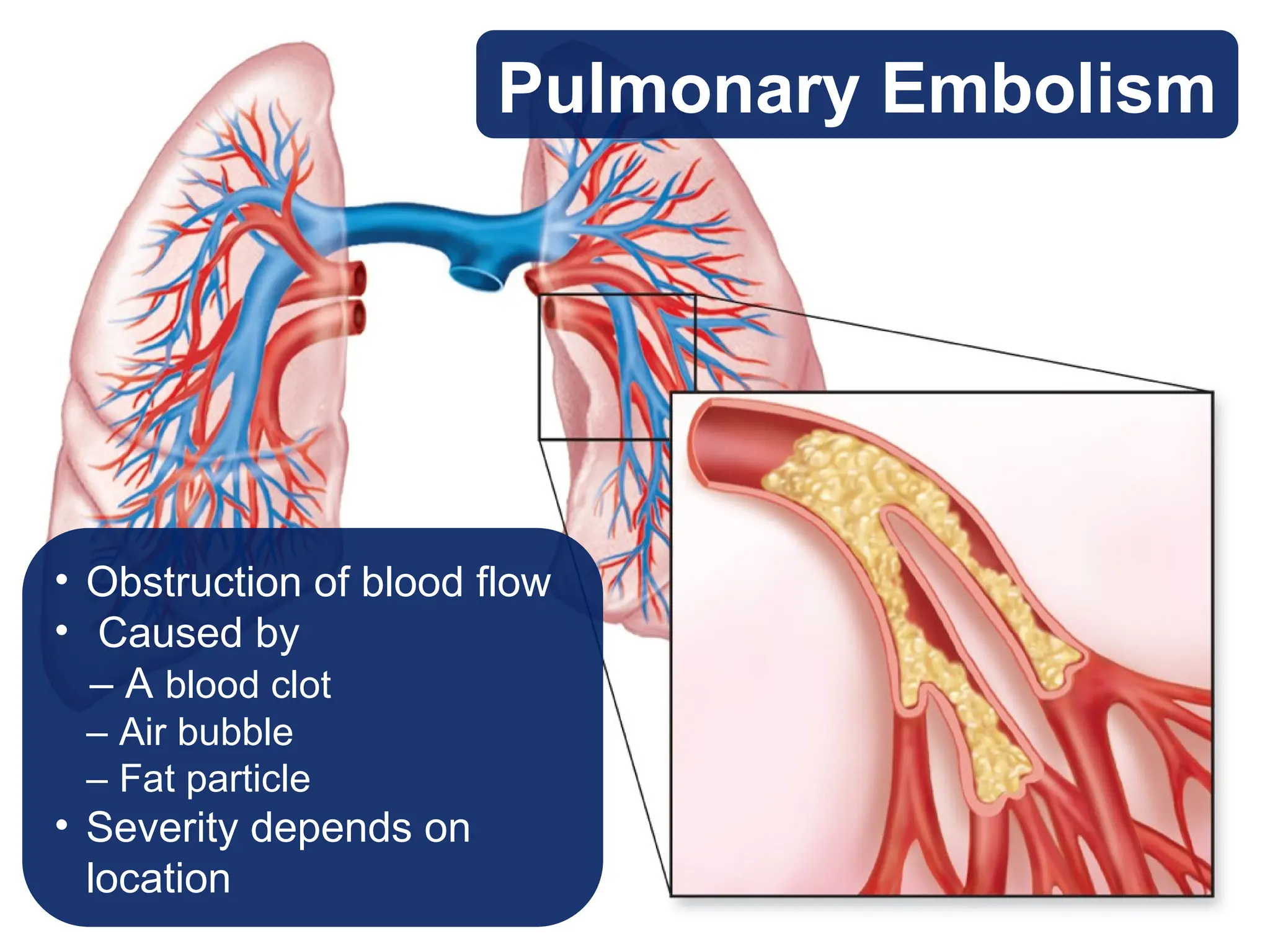
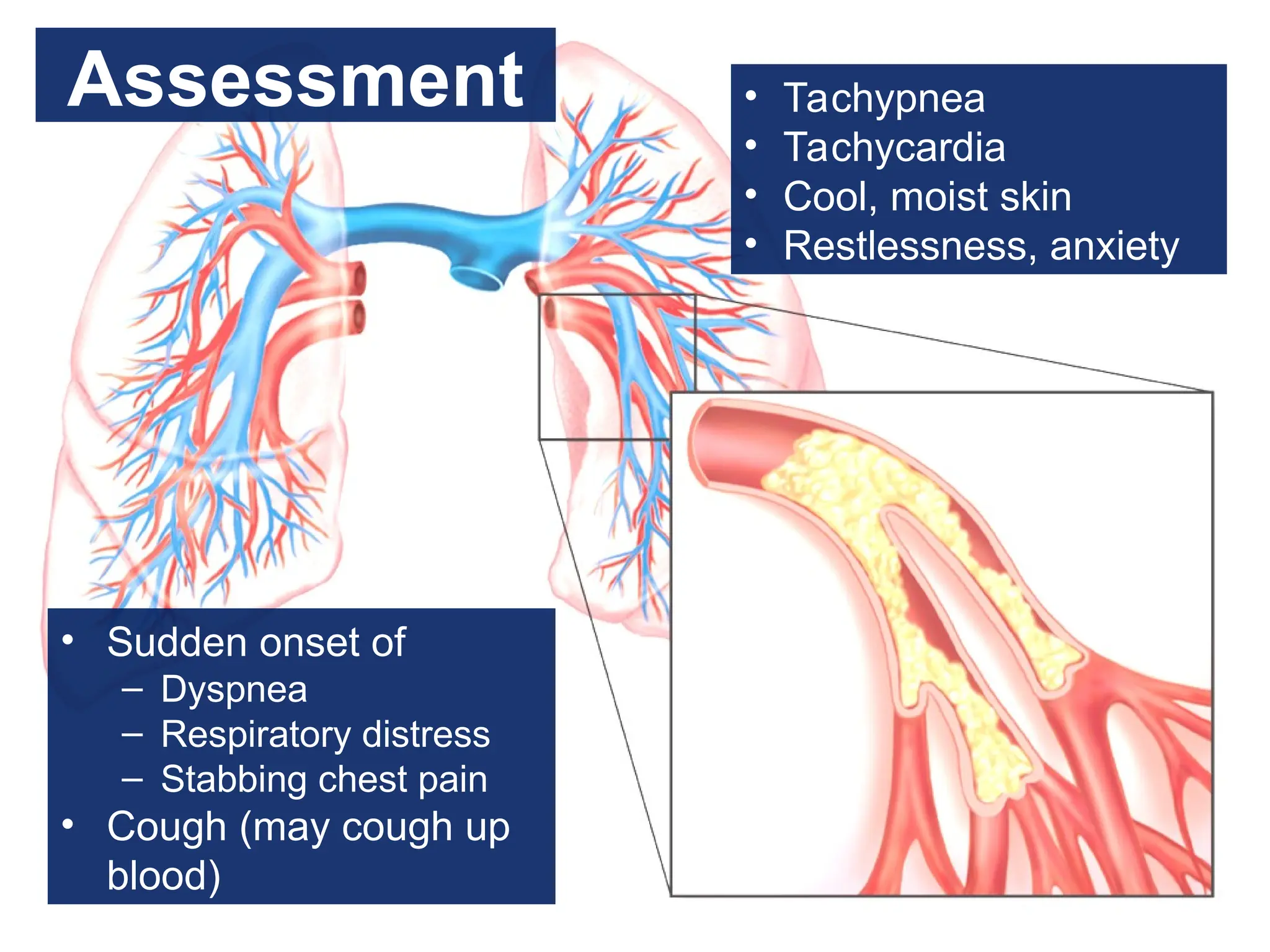
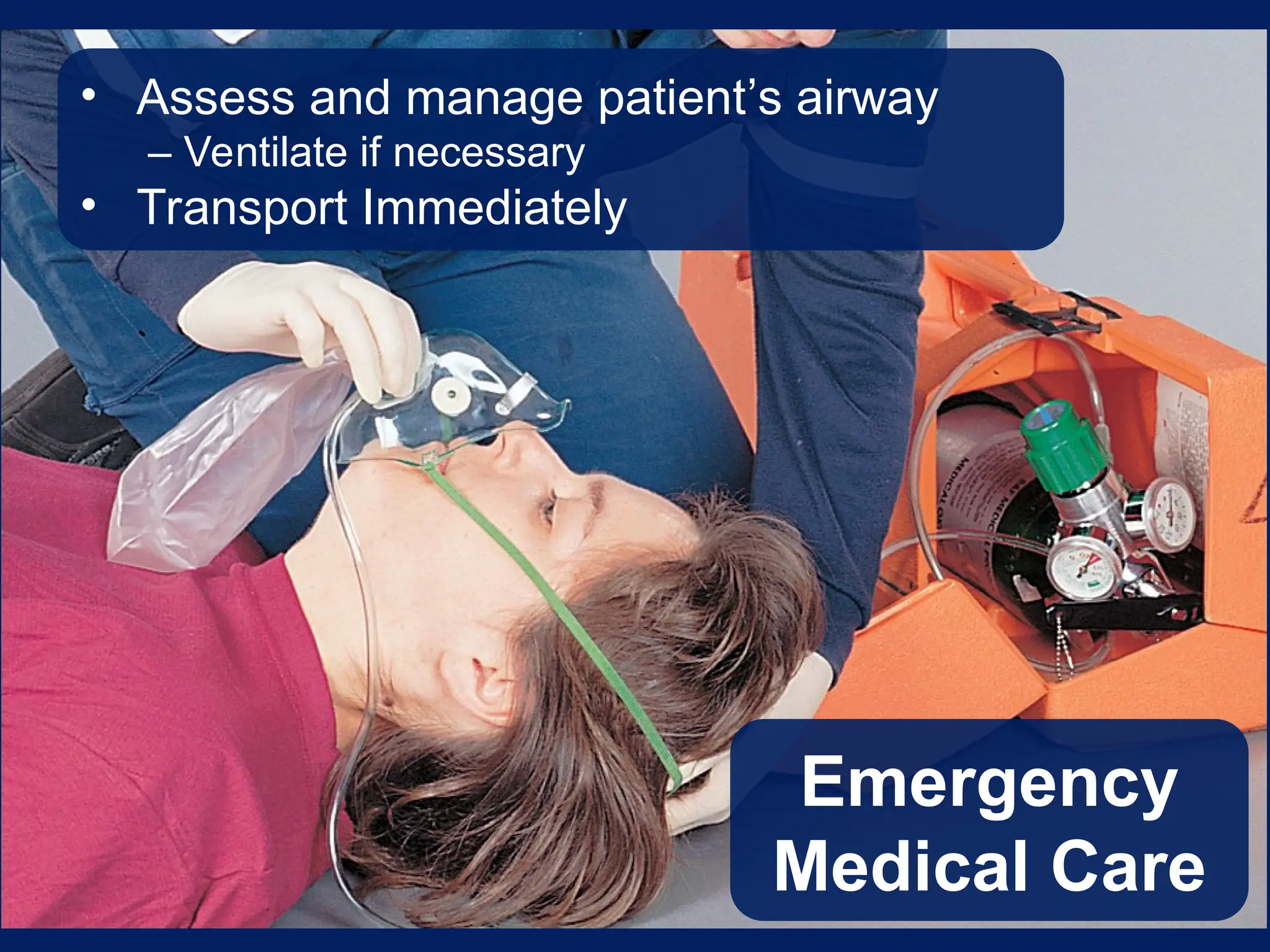
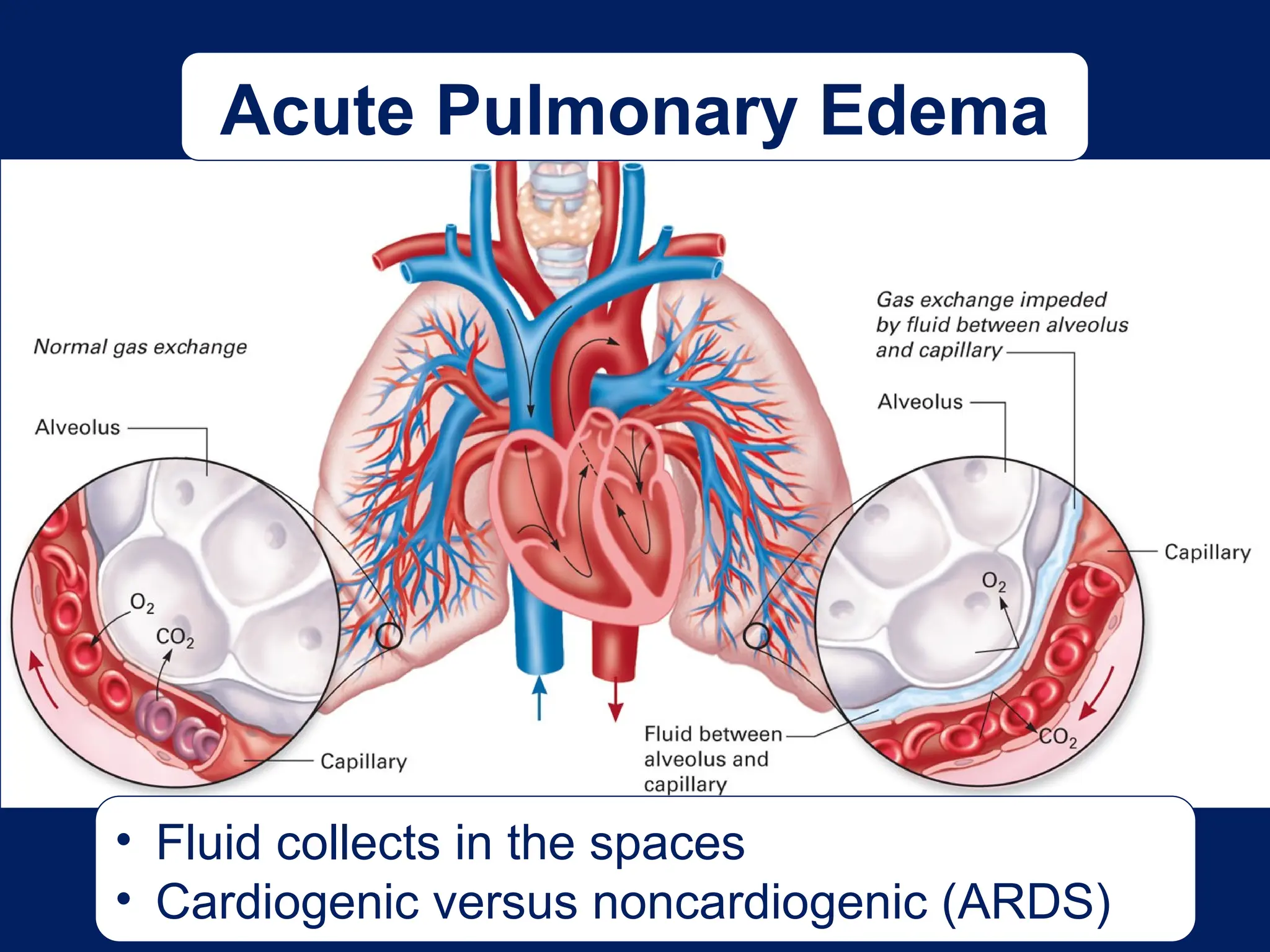
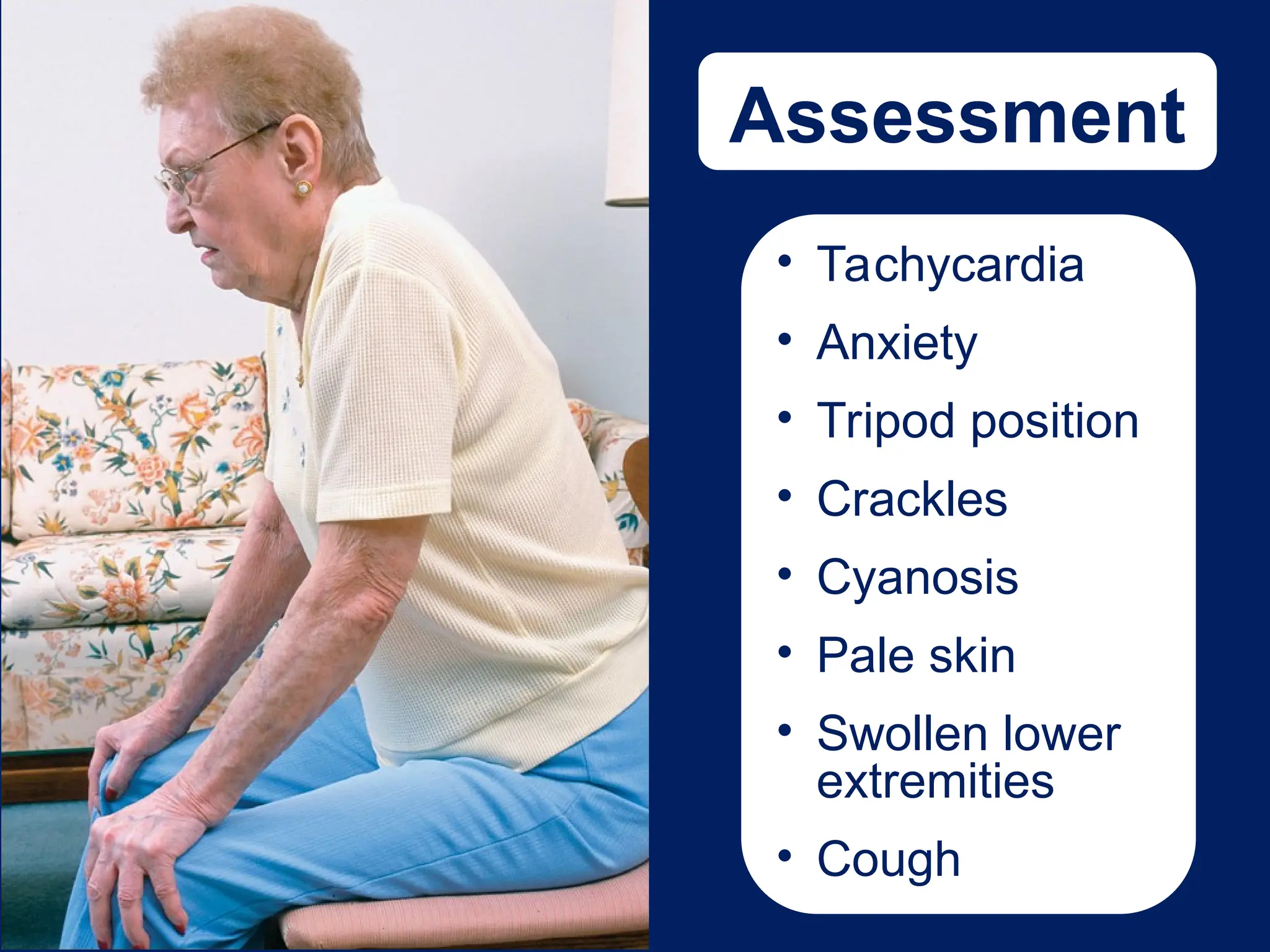
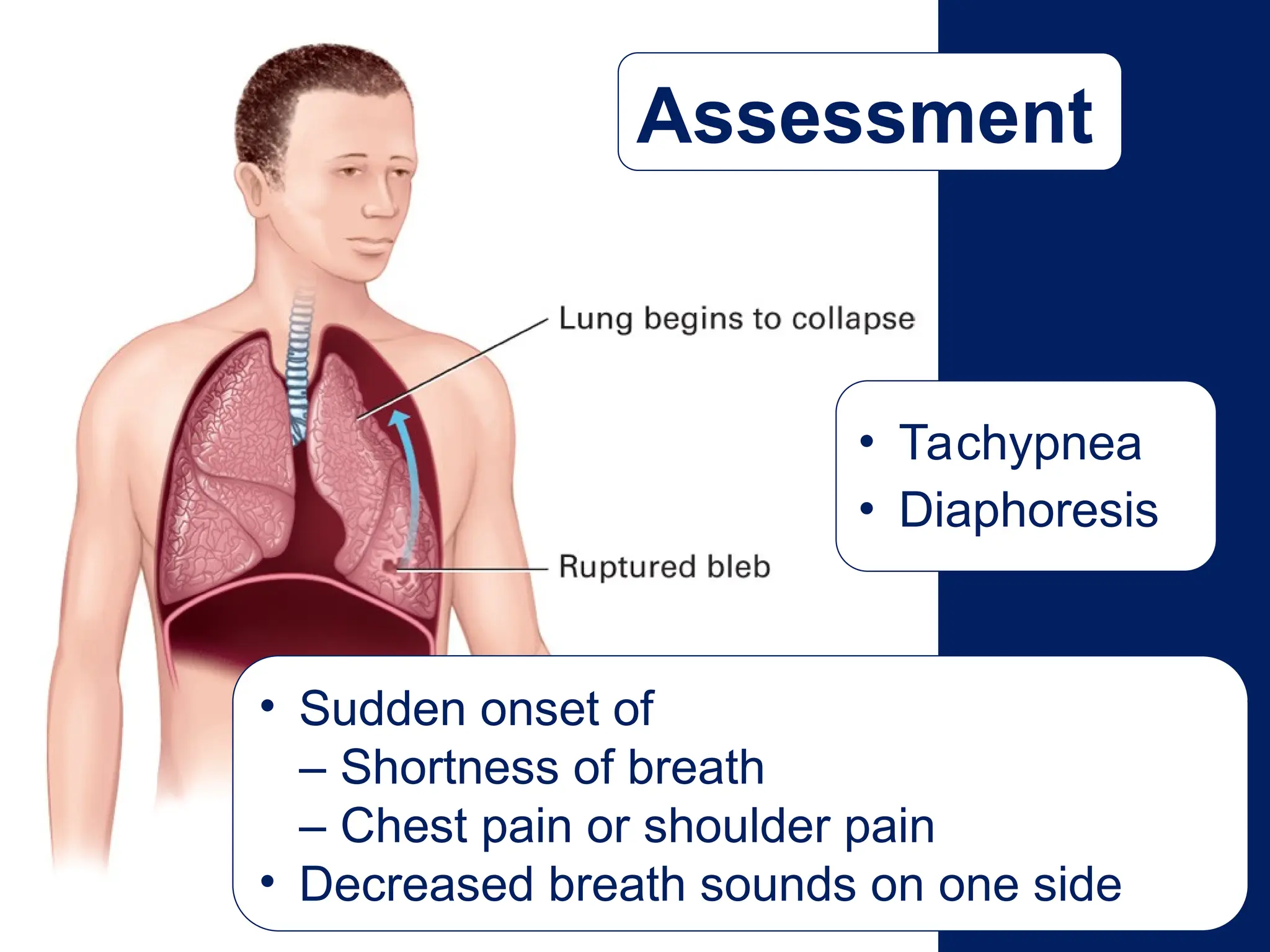
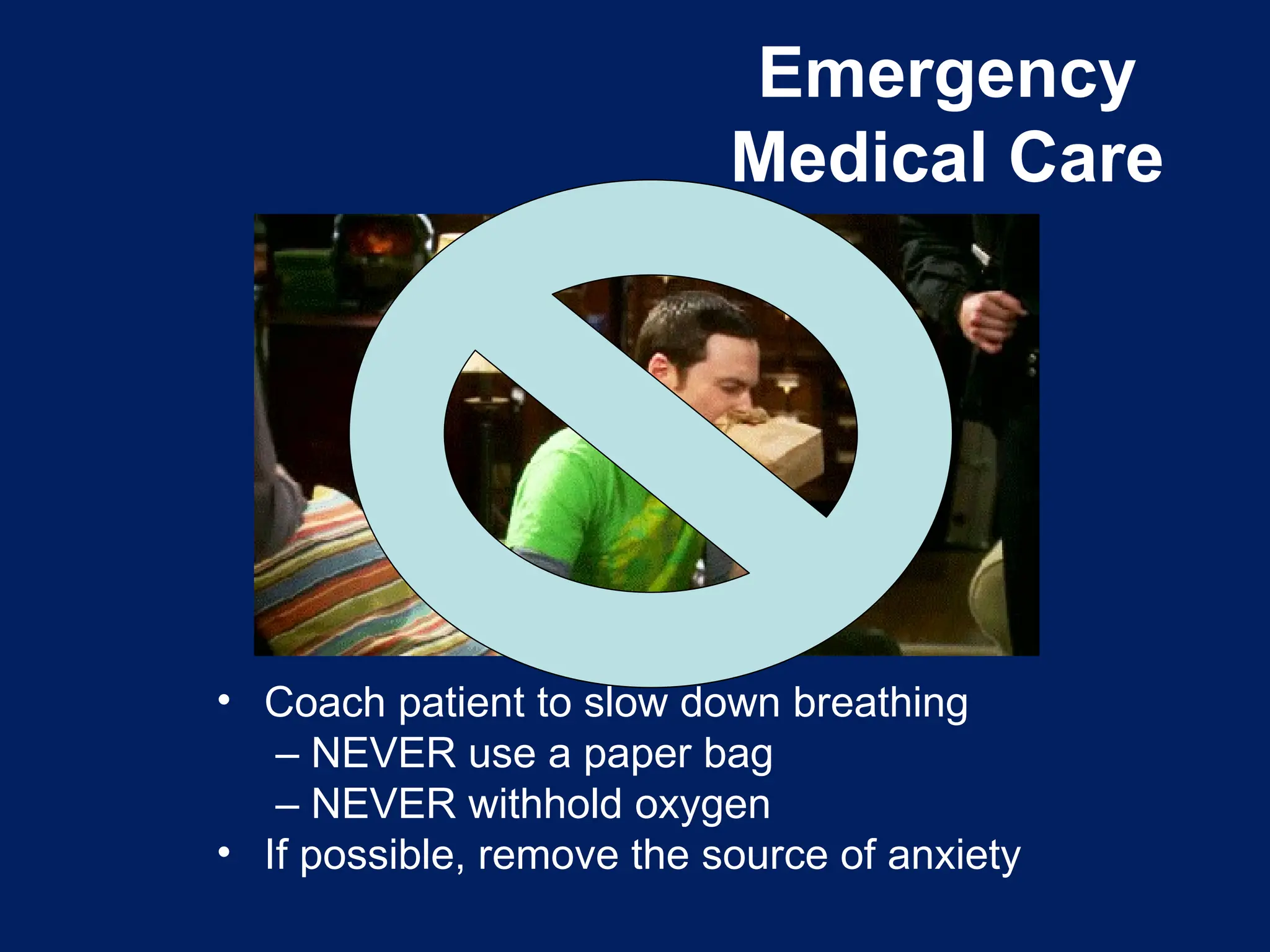
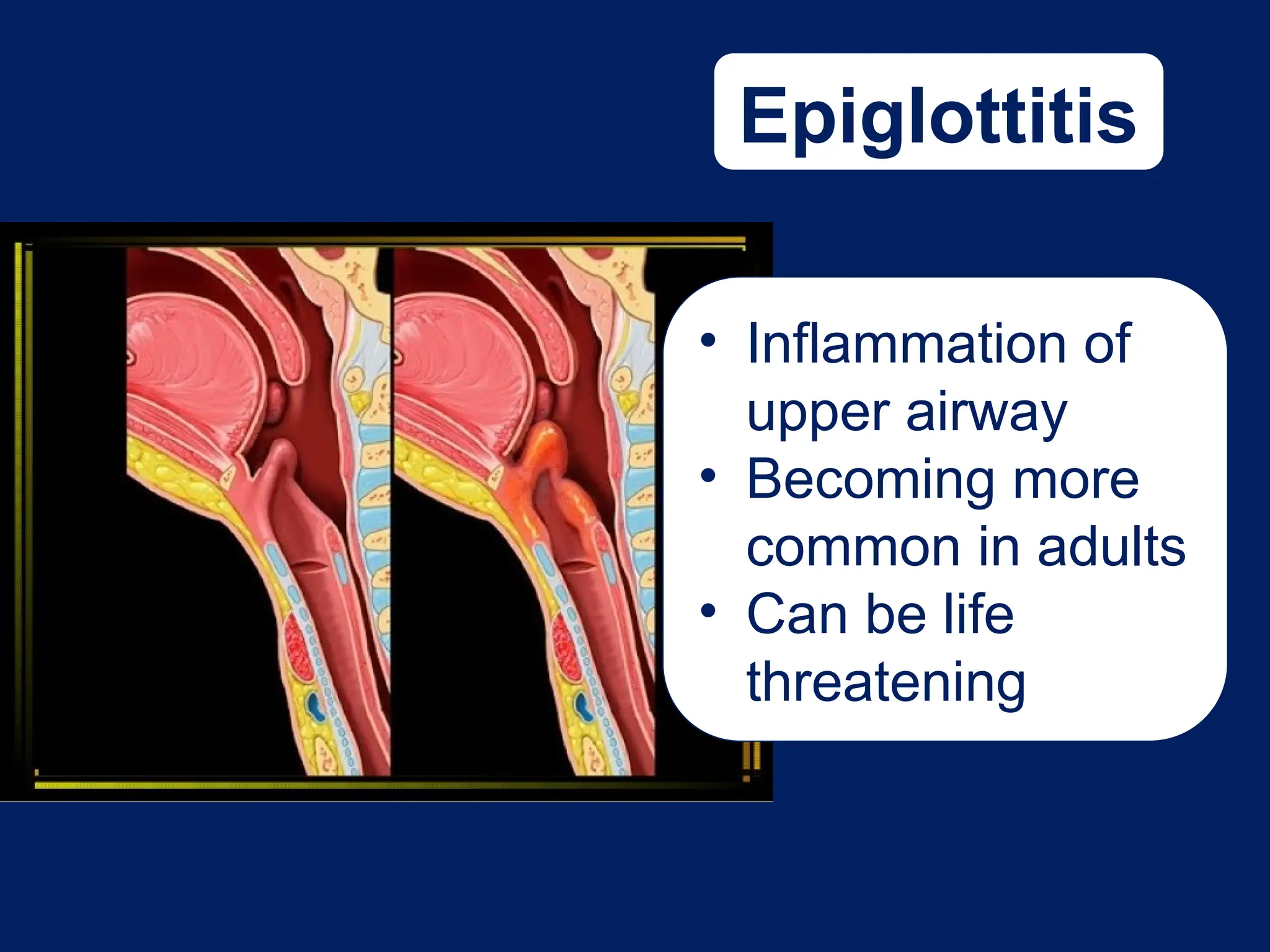
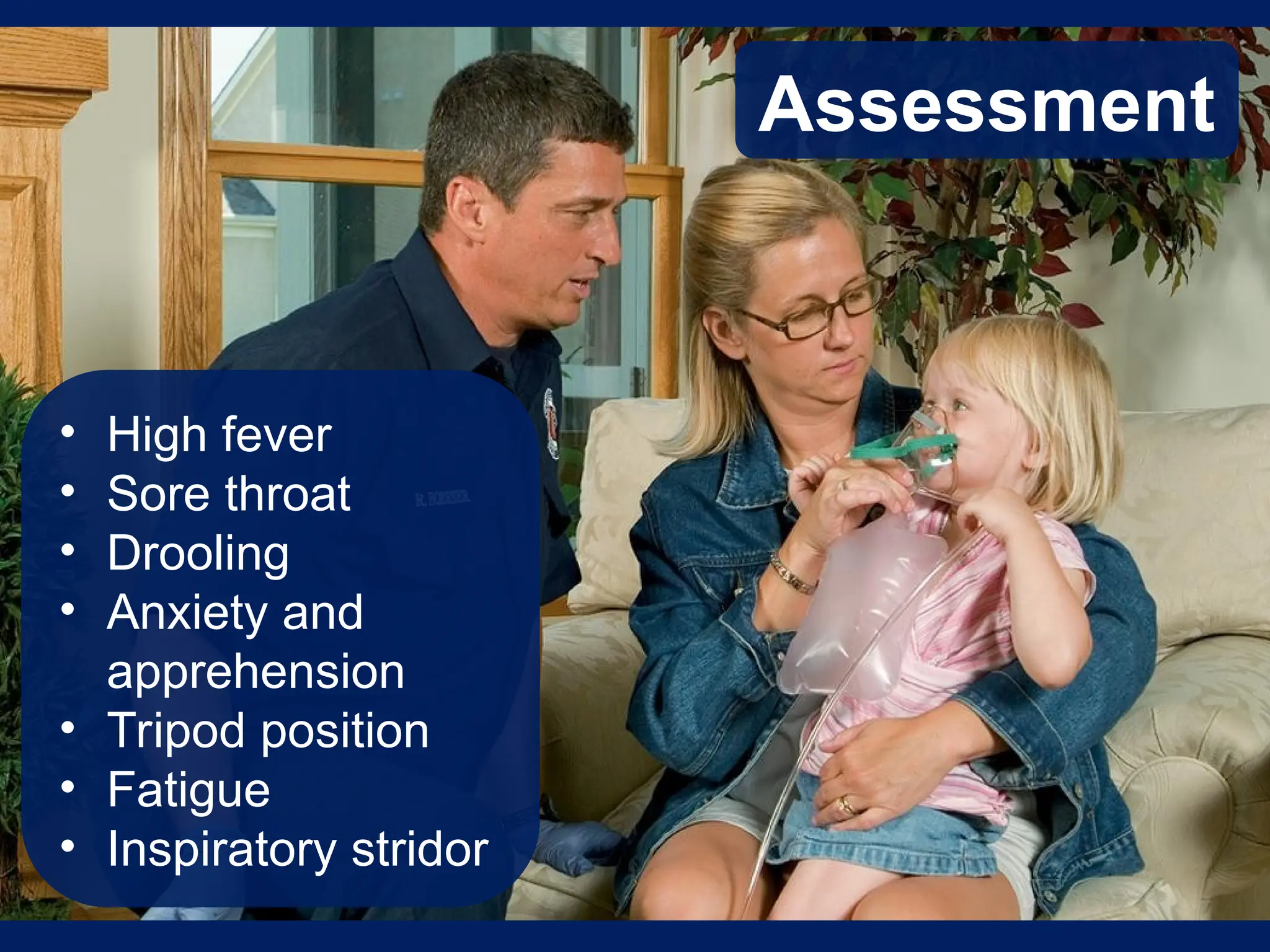
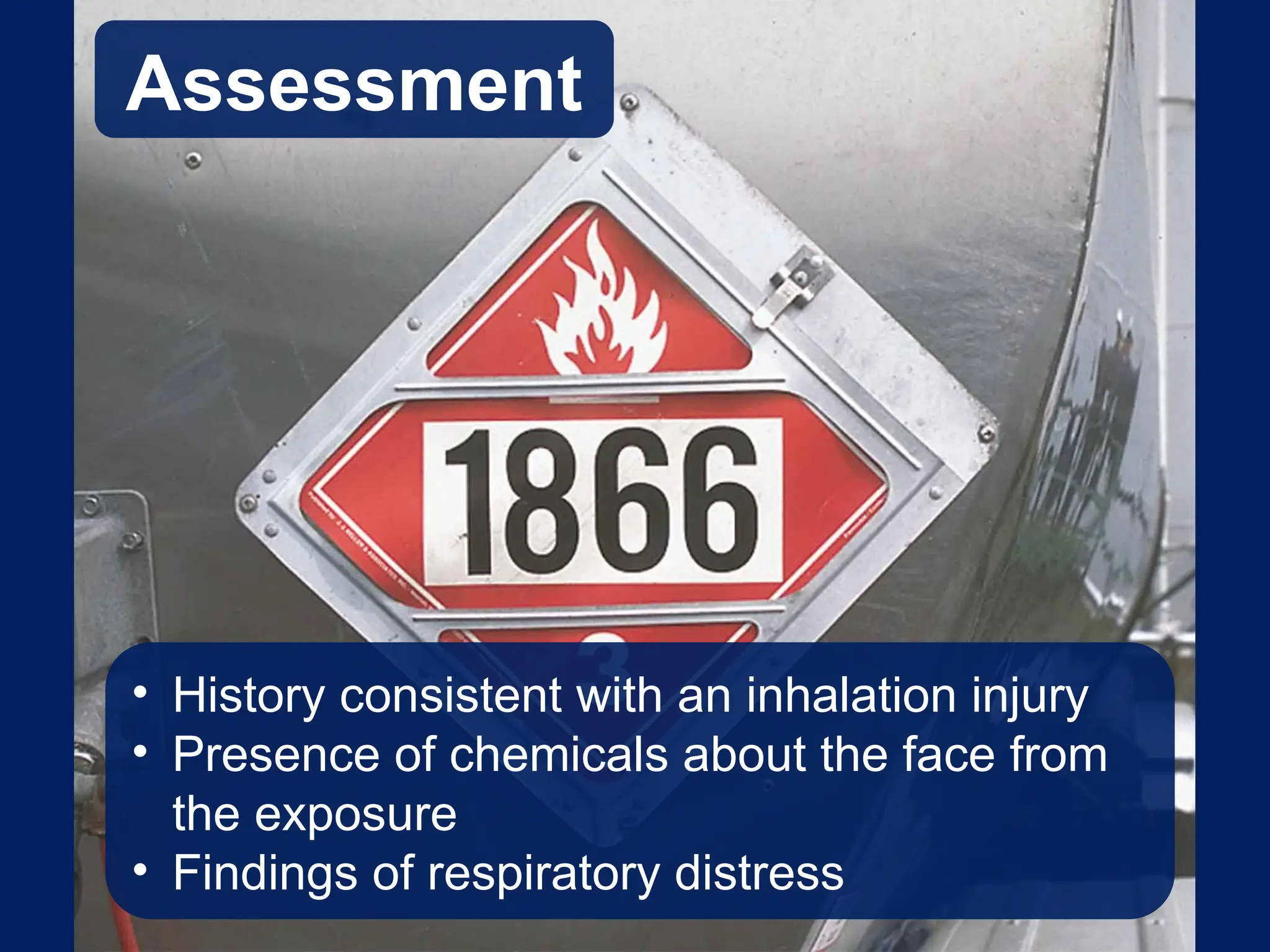
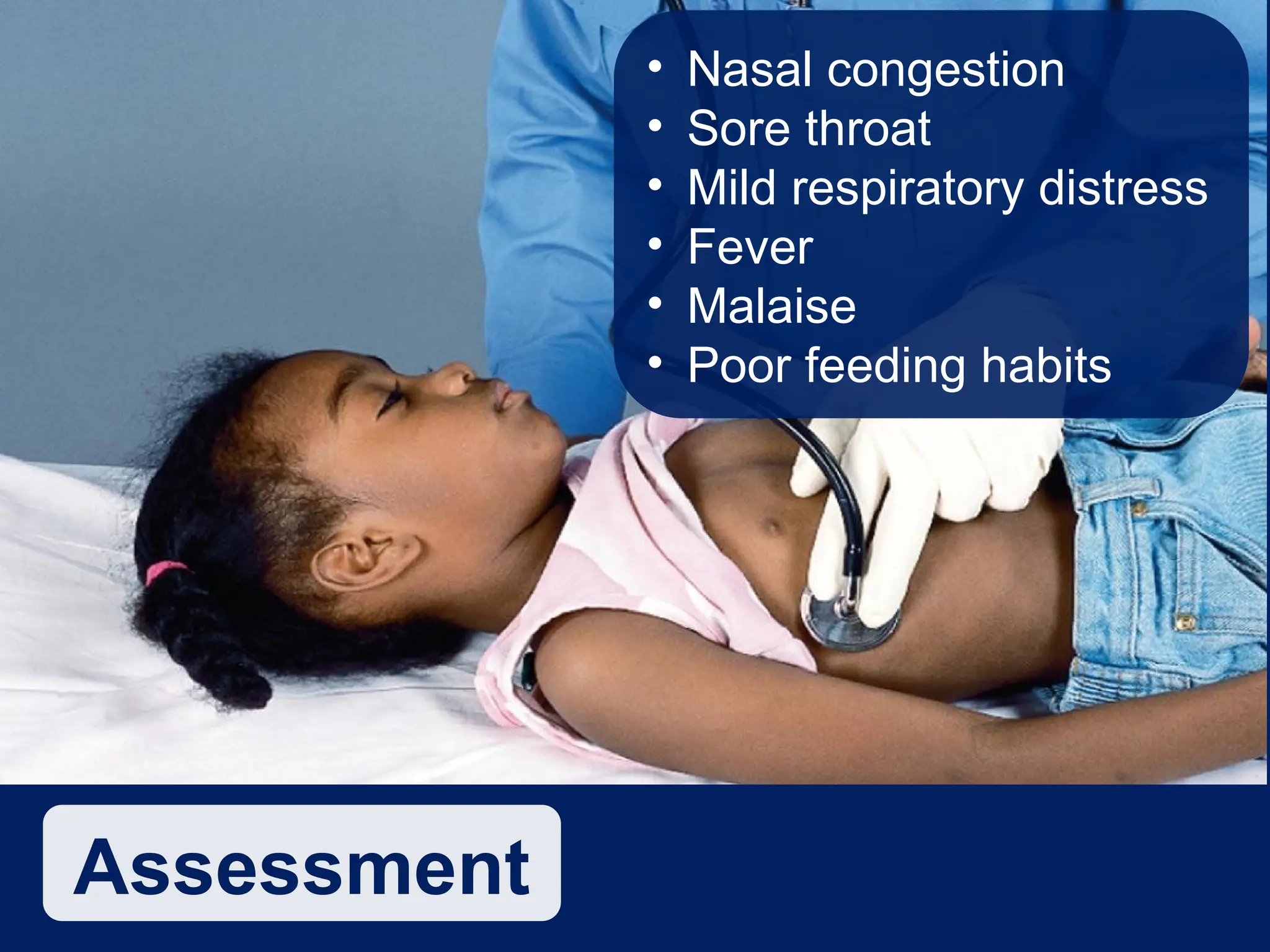
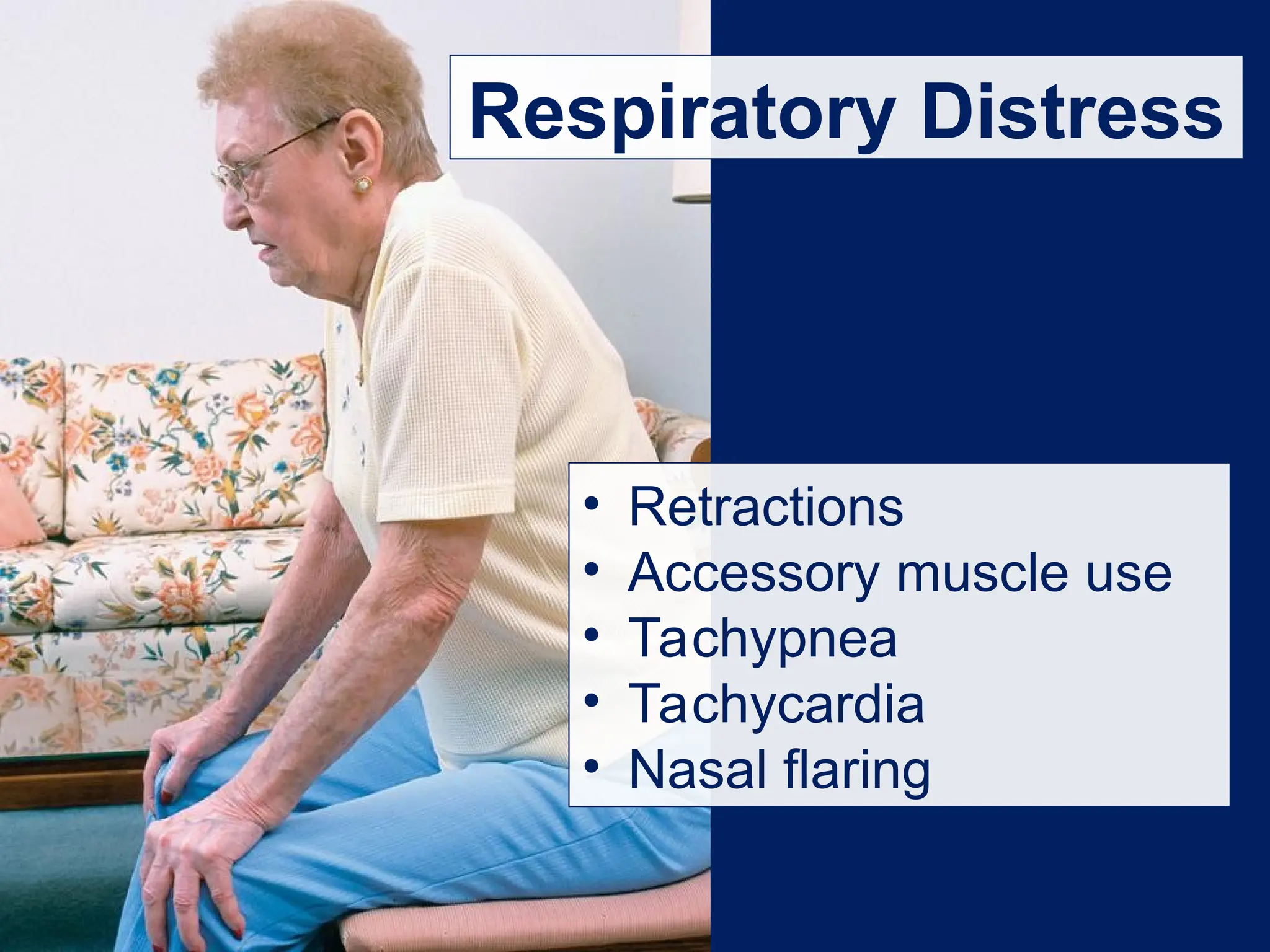
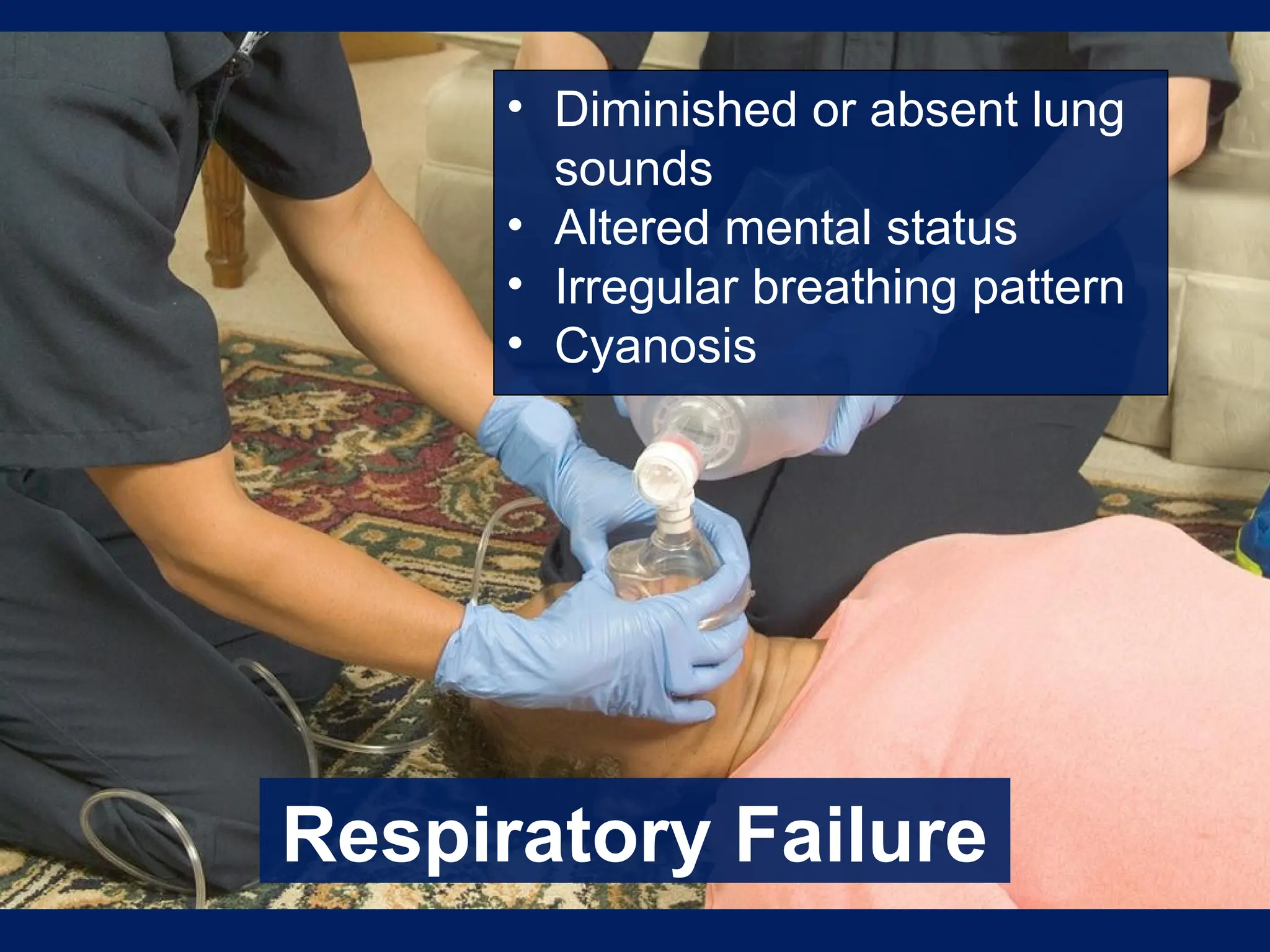
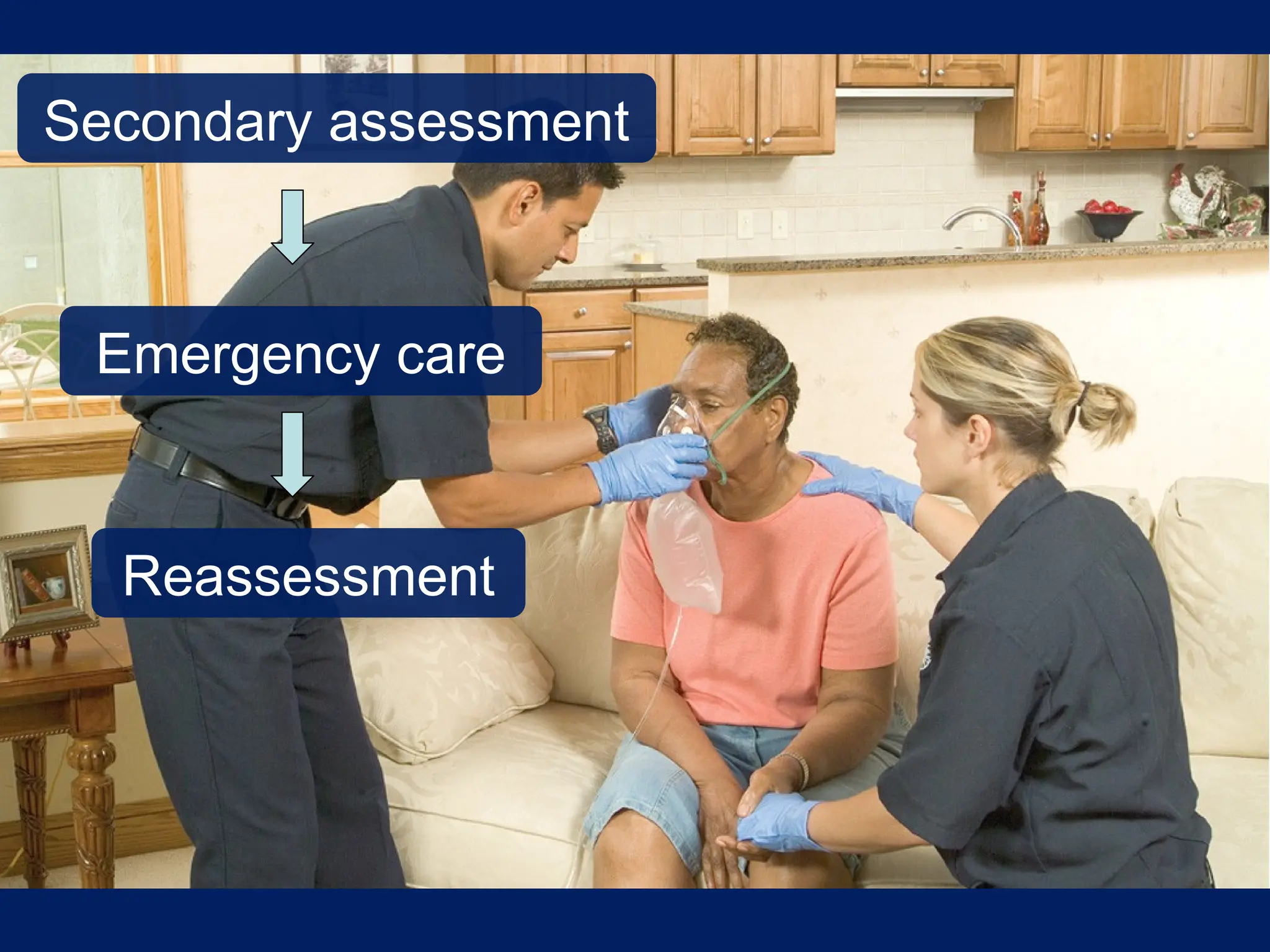
Chapter 16 covers respiratory emergencies, outlining the anatomy of the airway, the signs and symptoms of respiratory distress, and various conditions such as emphysema, chronic bronchitis, asthma, pneumonia, and pulmonary embolism. It emphasizes the importance of recognizing abnormal breathing patterns and understanding the appropriate emergency medical care for each condition, including the administration of oxygen and ventilatory support. The chapter also addresses age-related variations in respiratory assessments for pediatric and geriatric patients.