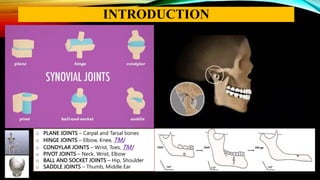
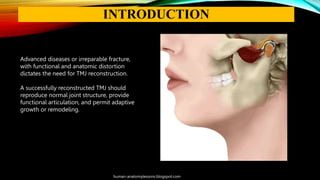
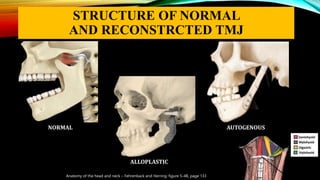
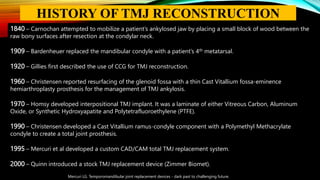
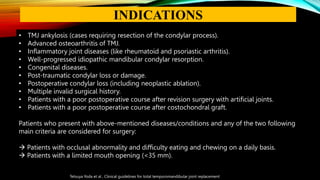
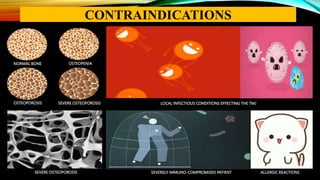
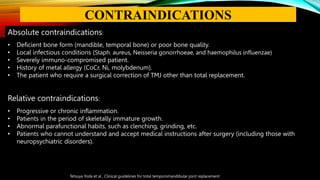
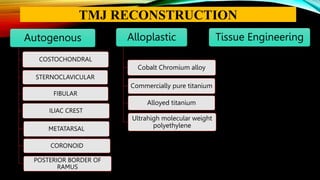
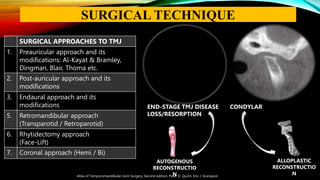
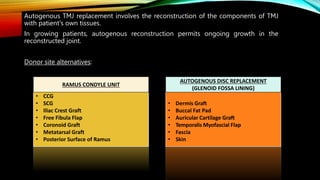
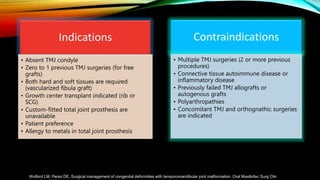
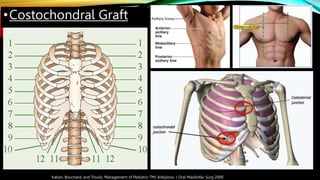
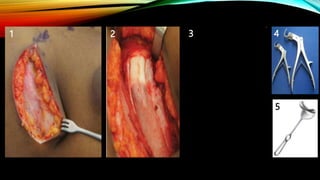
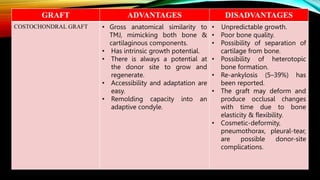
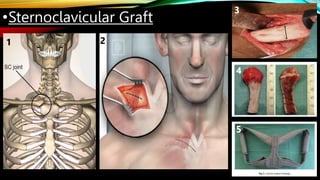
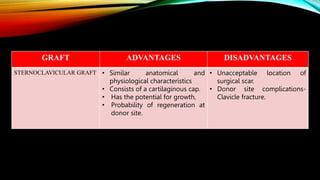
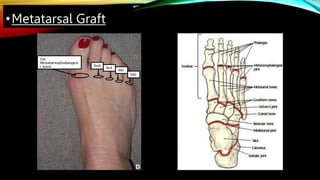
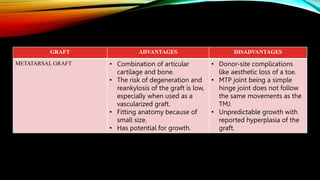
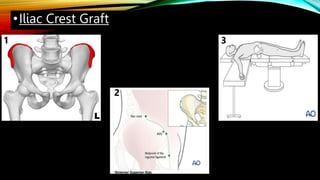
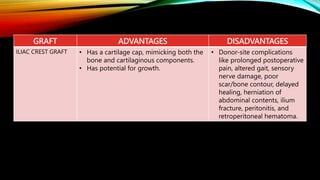
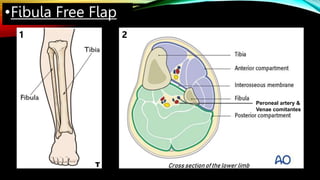
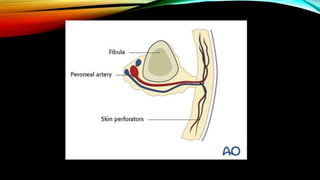
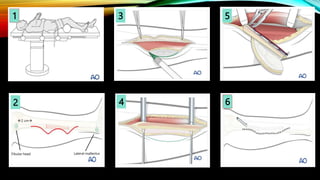
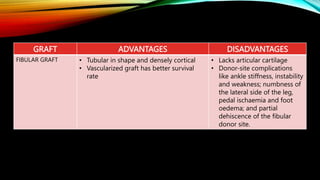
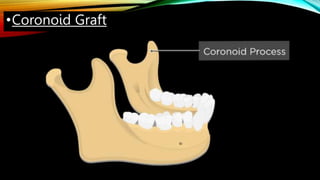
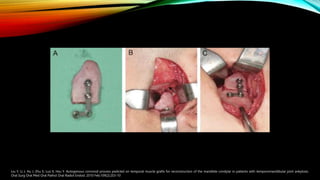
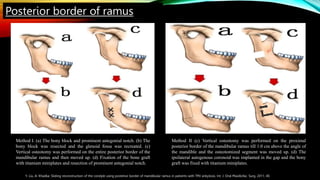
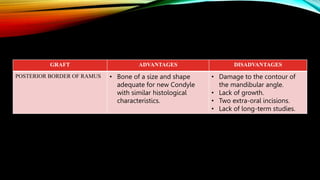
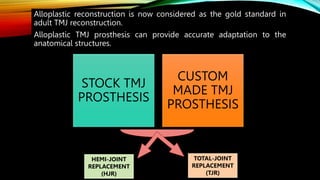
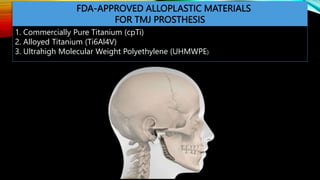
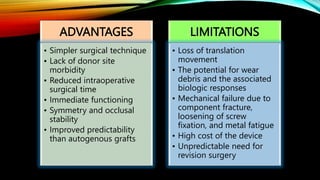
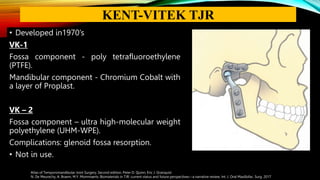
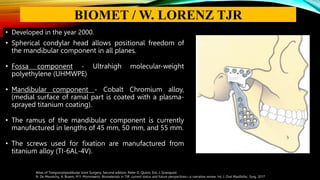
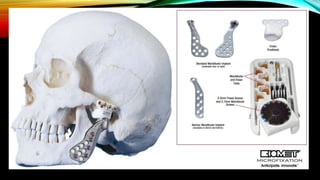
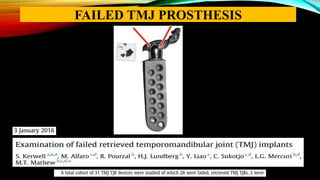
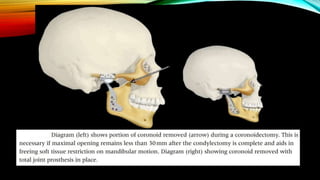
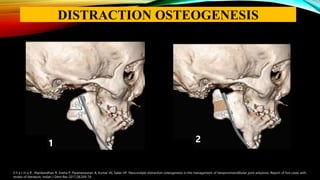
This document provides an overview of temporomandibular joint (TMJ) reconstruction techniques. It discusses the goals of TMJ reconstruction as restoring mandibular ramus length and morphology, an acceptable range of motion, and reestablishing normal jaw relations. Autogenous reconstruction uses the patient's own tissues and permits ongoing growth, while alloplastic reconstruction uses prosthetic devices. Common autogenous grafts discussed are costochondral, sternoclavicular, fibular, iliac crest, metatarsal, and coronoid grafts. Alloplastic options and a combined orthognathic approach are also summarized.