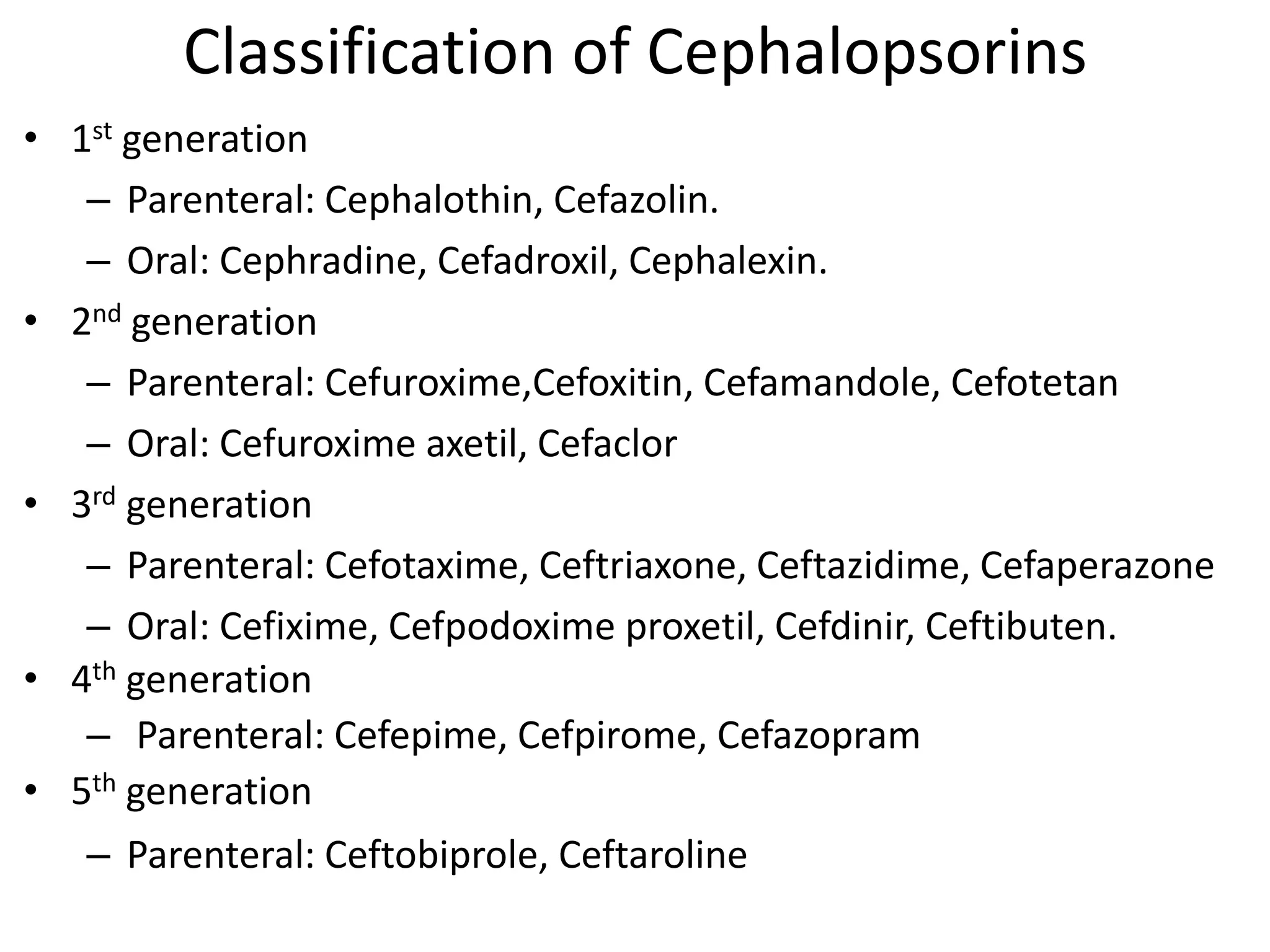
Cephalosporins are a class of semisynthetic, β-lactam antibiotics derived from the fungus Cephalosporium. They are classified into 5 generations based on their year of development and spectrum of activity. Cephalosporins work by inhibiting bacterial cell wall synthesis through binding to penicillin-binding proteins and preventing transpeptidation and cross-linking of peptidoglycan chains. This results in cell lysis and a bactericidal effect. Later generations have increased activity against Gram-negative bacteria and β-lactamase producers. Common uses include respiratory, urinary, skin/soft tissue infections as well as meningitis. Adverse effects are generally mild and include hyper