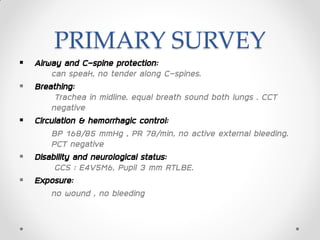
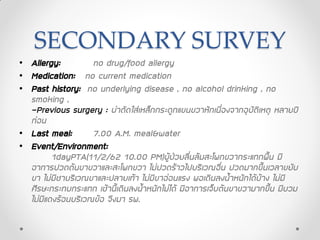
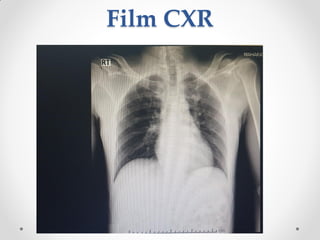
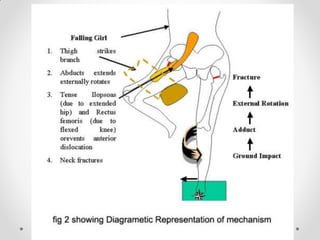
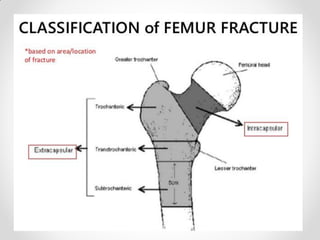
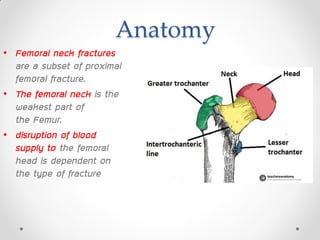
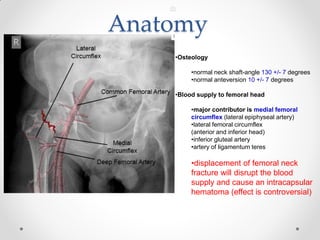
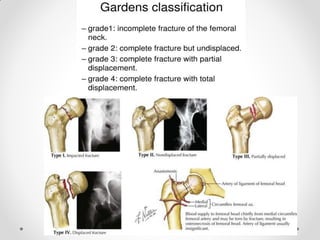
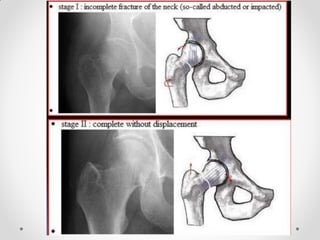
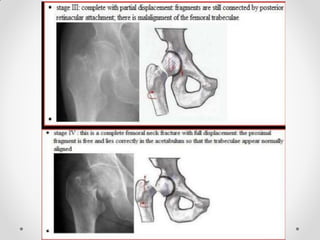
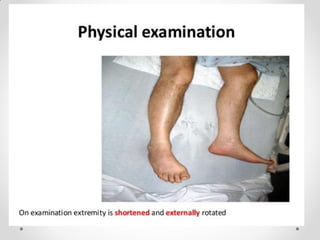
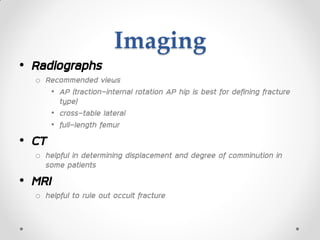
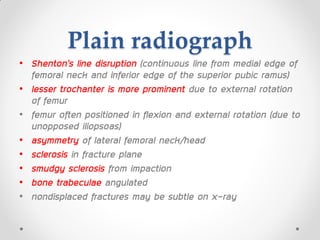
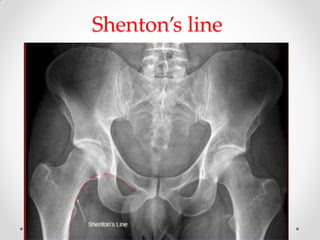
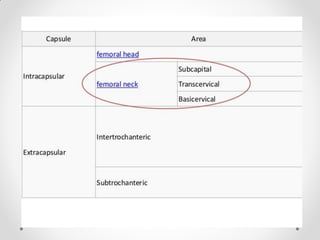
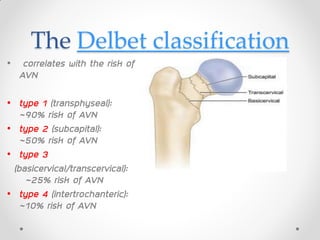
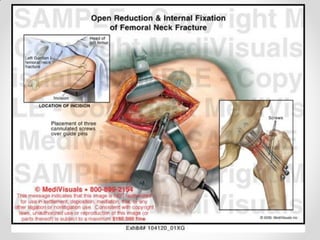
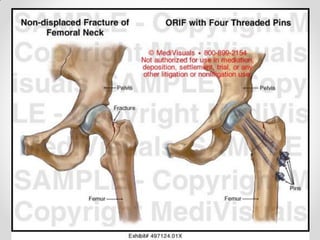
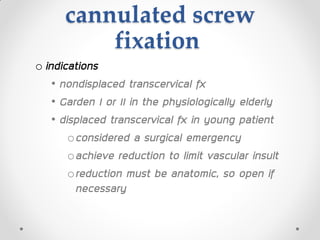
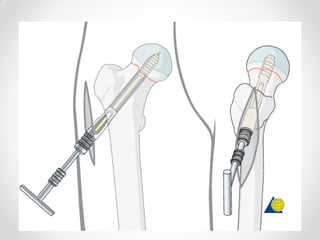
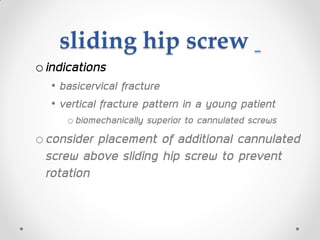
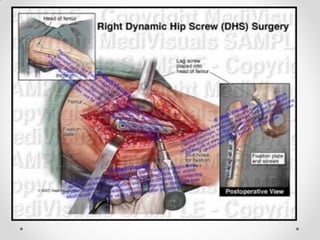
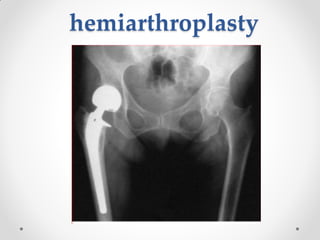
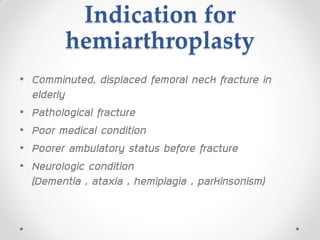
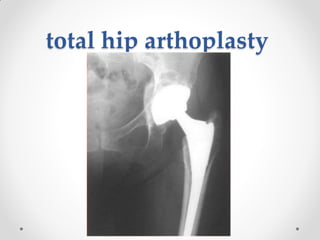
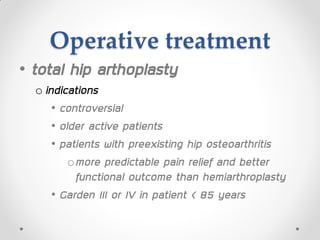
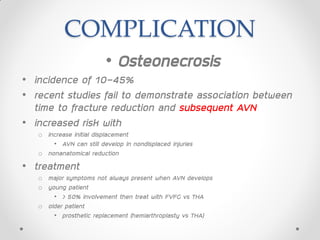
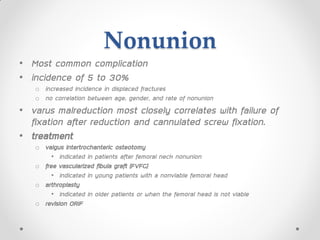
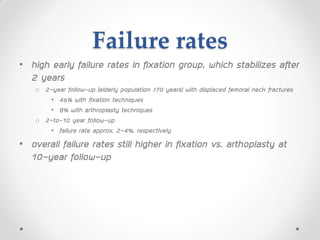
This case conference discusses a 48-year-old Thai man who presented to the hospital after falling and injuring his right hip. On examination, he had tenderness and swelling of the right hip and thigh with limited range of motion due to pain. X-rays revealed a closed fracture of the right femoral neck. The attending physician provided a provisional diagnosis and treatment plan involving admission, skin traction, pain medication, and monitoring. The discussion then reviewed femoral neck fractures, including risk factors, mechanisms of injury, imaging, classifications, complications, and treatment options such as internal fixation, hemiarthroplasty, or total hip arthroplasty.