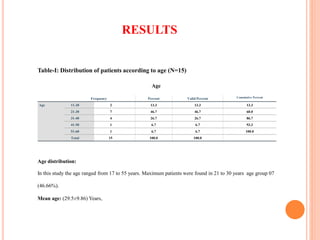
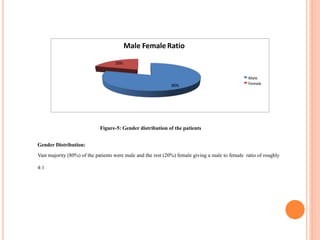
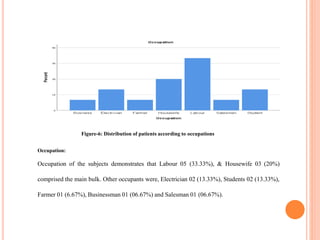
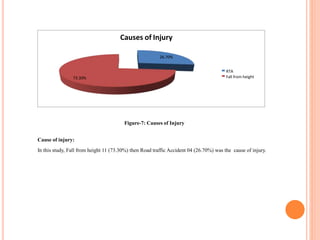
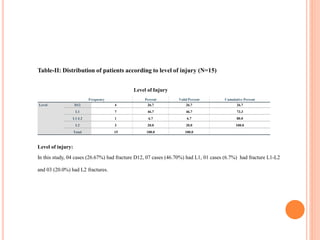
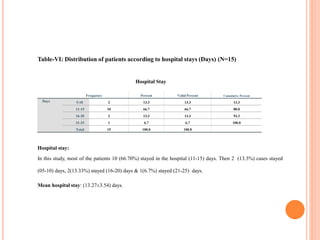
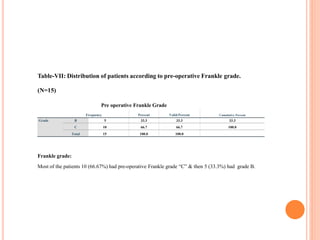
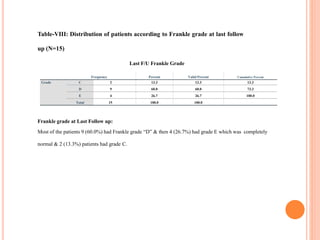
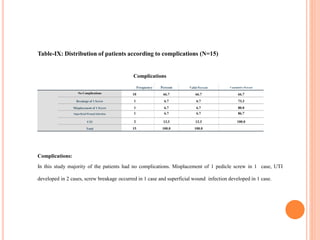
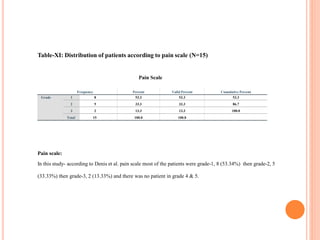
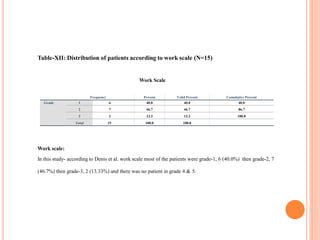
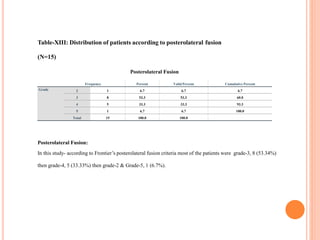
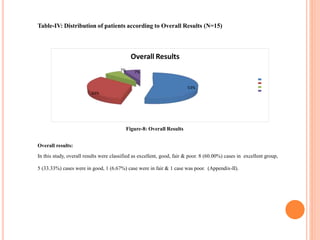
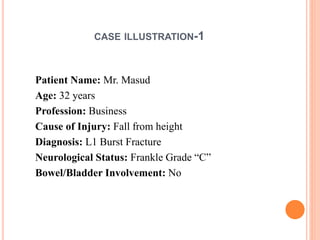
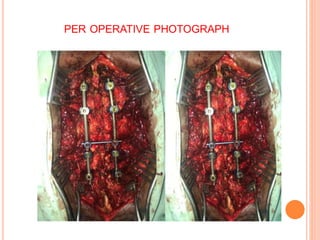
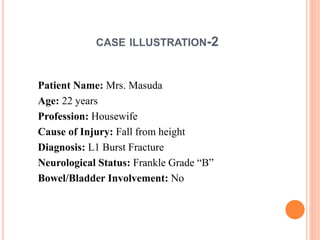
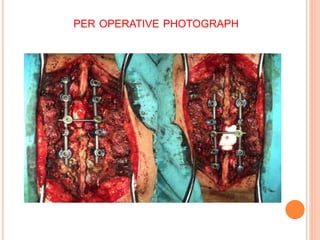
This study evaluated the functional outcomes of 15 patients who underwent thoracolumbar burst fracture stabilization using pedicle screw fixation and rods. Most patients were males between 21-30 years old, with falls being the primary cause of injury. The L1 vertebrae was most commonly fractured. Post-operatively, most patients experienced reduced pain and improved mobility, with 86.66% showing excellent or good functional outcomes and a mean hospital stay of 13 days. The results demonstrate pedicle screw fixation to be an effective procedure for stabilizing thoracolumbar burst fractures.