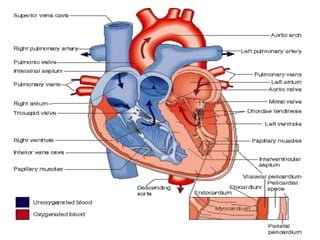
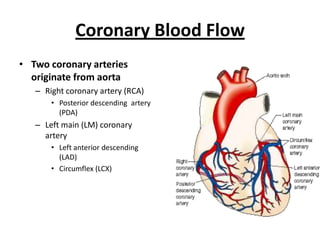
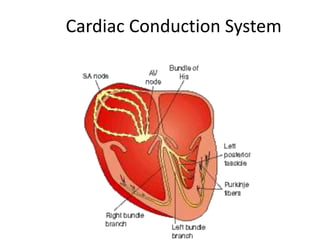
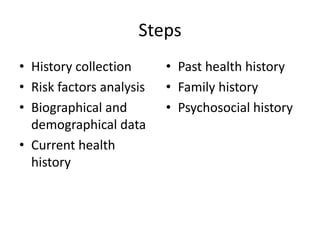
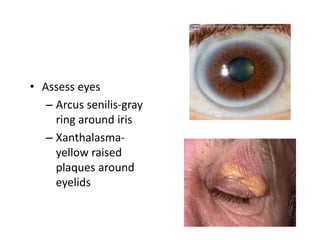
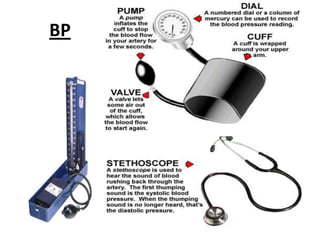
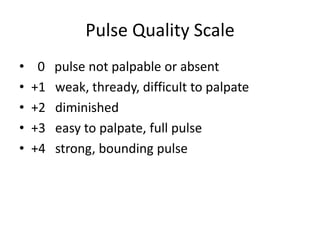
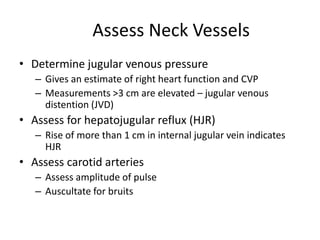
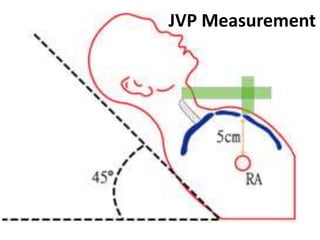
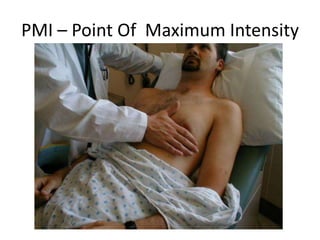
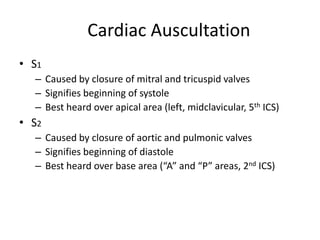
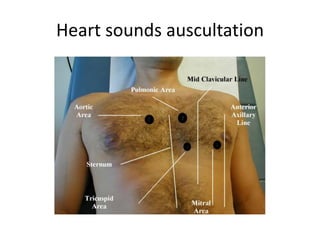
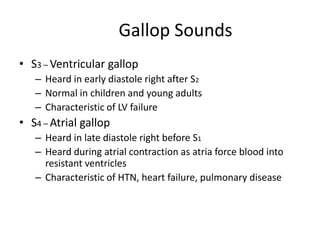
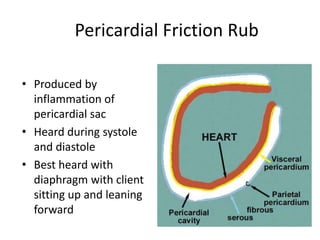
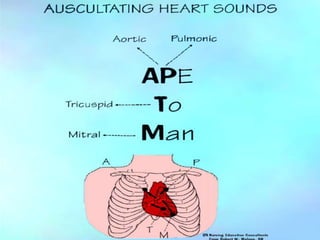
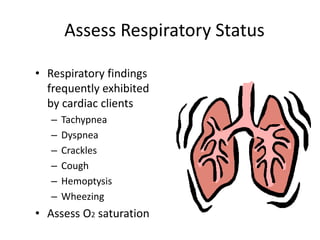
This document provides an overview of cardiac anatomy, physiology, and assessment. It begins with a description of the heart's structure including the coronary arteries and conduction system. Key concepts are explained such as the cardiac cycle, output, and factors that determine stroke volume like preload, afterload, and contractility. Common symptoms of cardiovascular disease are outlined. The document then details the steps and focus of a cardiac assessment including gathering a health history and examining vital signs, skin, neck, heart, lungs, and abdomen. Potential exam findings and complications are also noted.