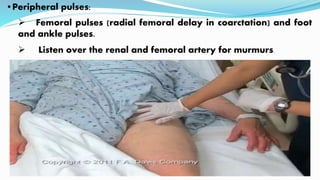
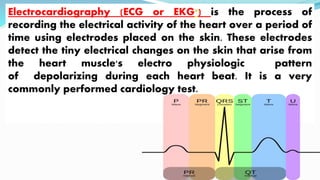
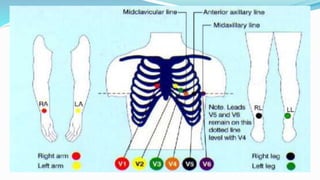
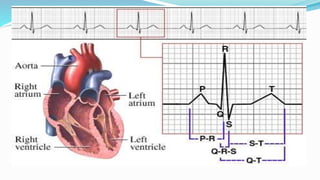
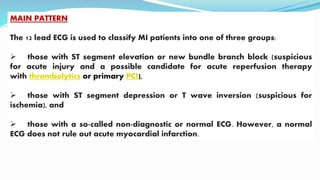
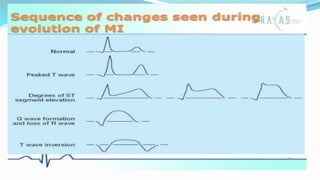
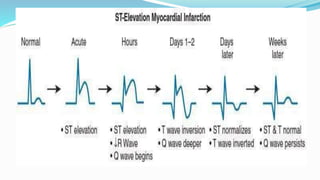
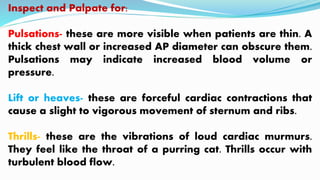
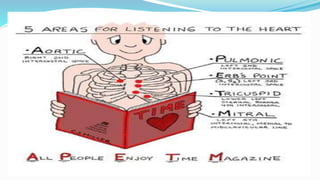
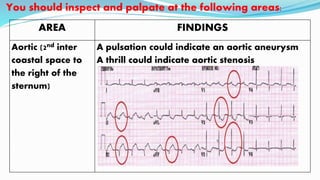
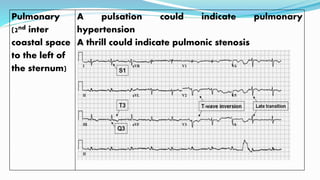
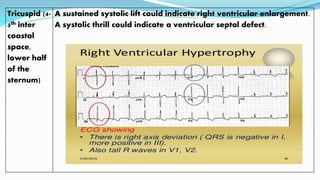
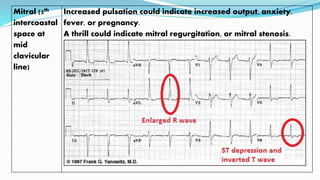
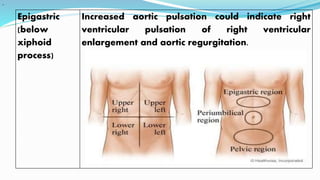
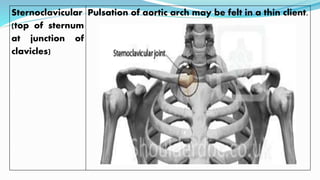
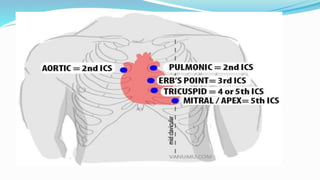
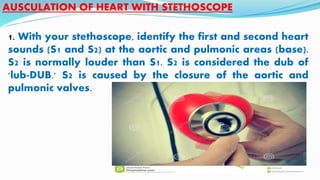
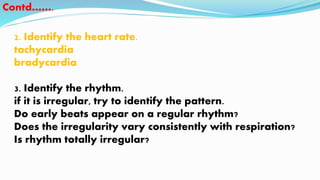
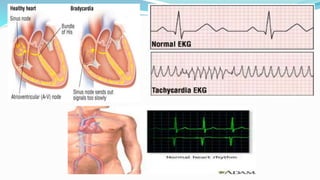
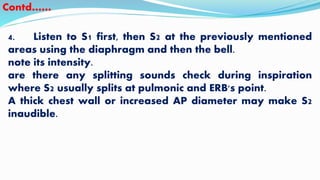
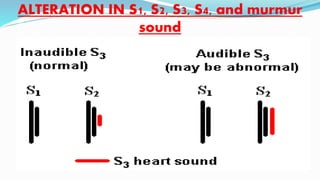
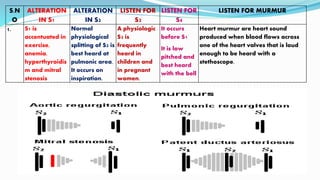
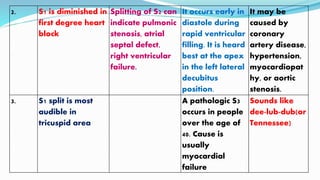
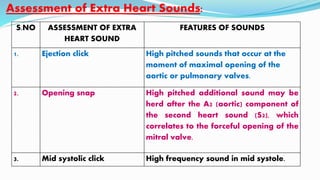
This document provides guidance on assessing the cardiovascular system through physical examination. It describes how to inspect general appearance, check for cyanosis, examine the face, hands, pulse, blood pressure, chest, abdomen, and other areas. It also discusses auscultating heart sounds at various locations and what alterations may indicate, as well as investigating with electrocardiography, echocardiography, and other tests. Physical assessment of the cardiovascular system is important for evaluating a patient's condition, documenting findings, and guiding treatment and care.