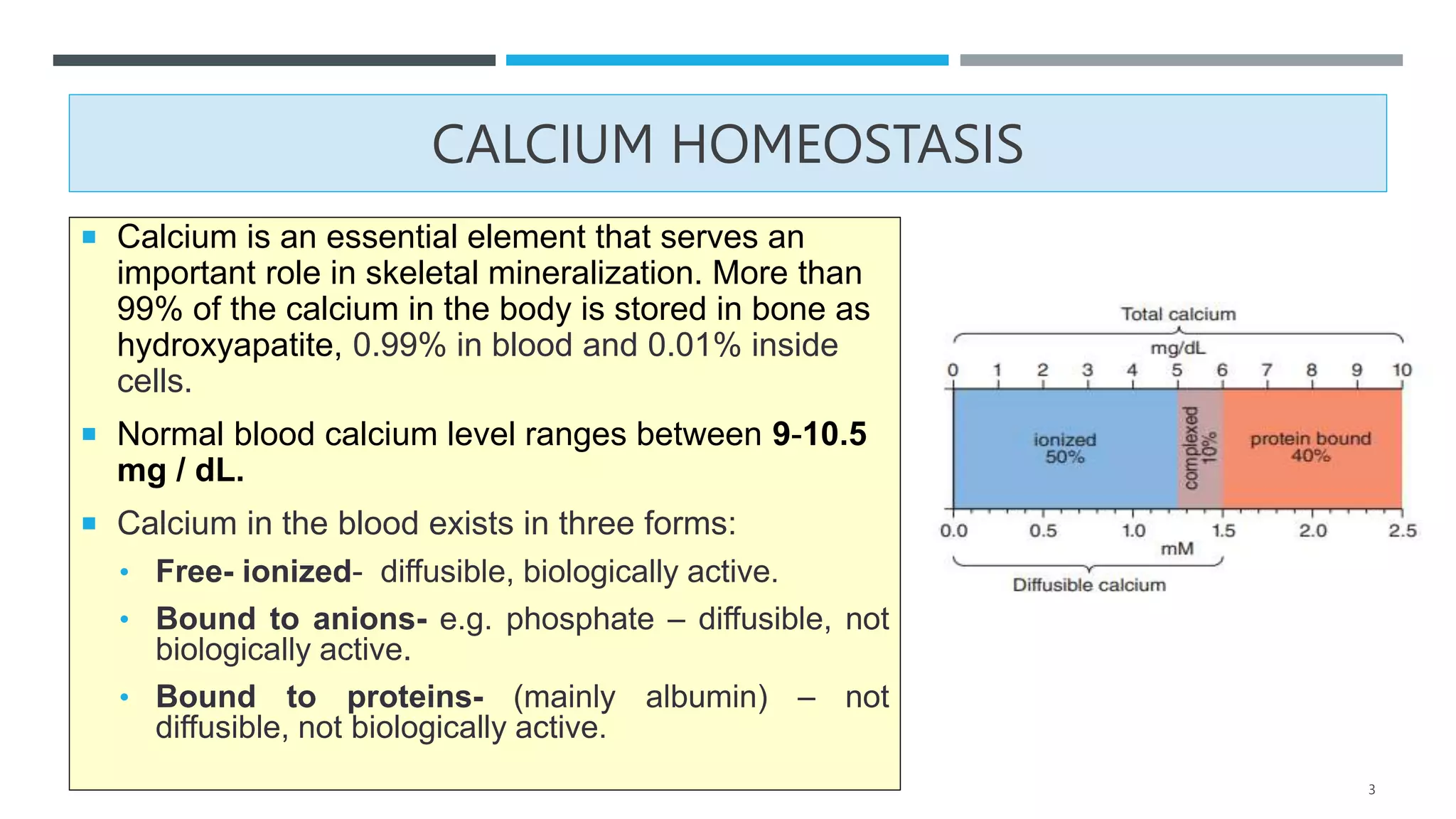
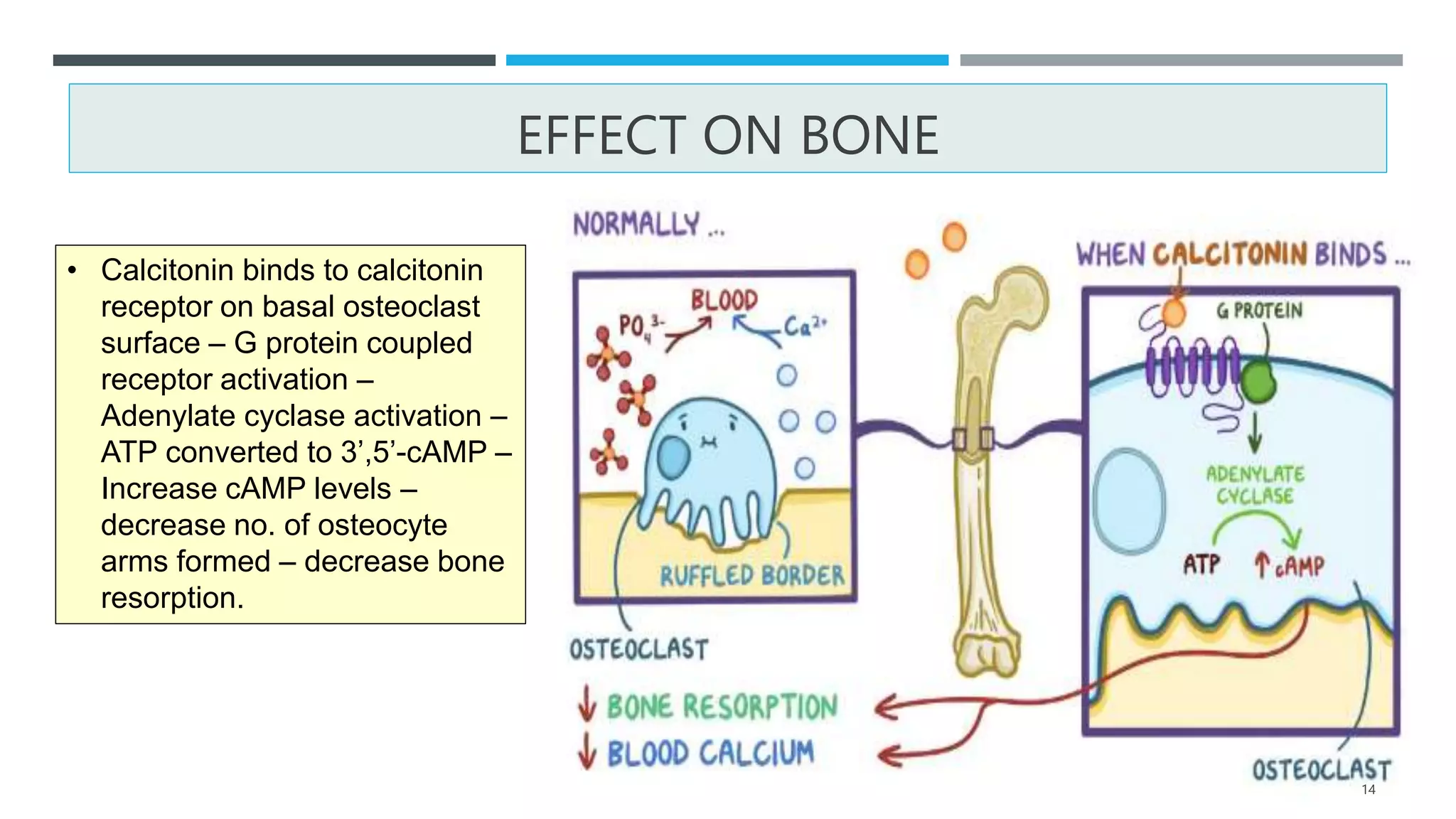
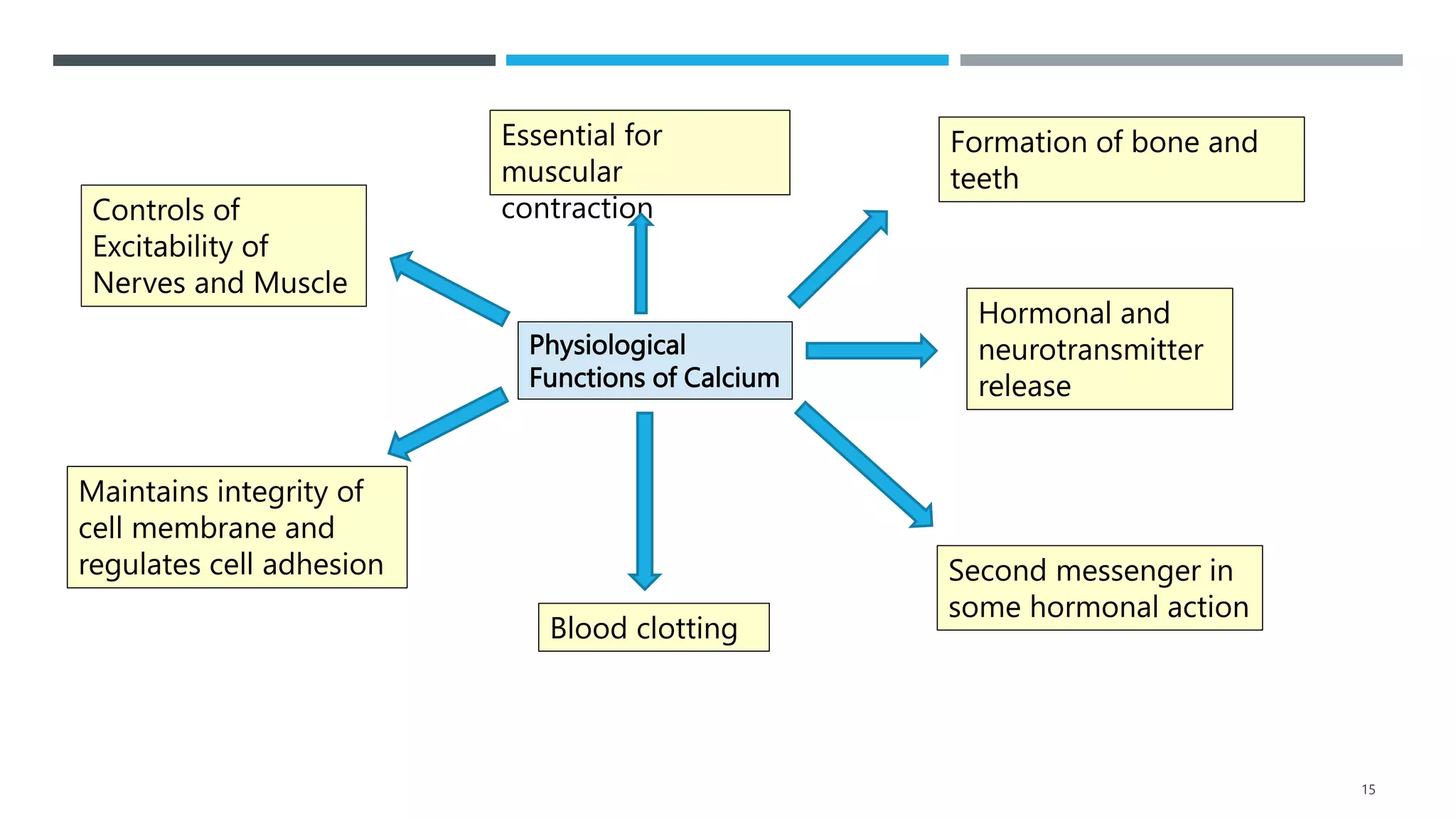
This document summarizes calcium regulation and the hormones involved - Parathyroid hormone (PTH), Vitamin D, and Calcitonin. PTH increases blood calcium levels by promoting bone resorption and calcium reabsorption in the kidneys. Vitamin D helps absorb calcium in the intestines and reabsorb it from bone. Calcitonin decreases blood calcium levels by inhibiting bone resorption and calcium reabsorption in the kidneys. Together these hormones tightly control calcium homeostasis and levels in the blood and bones.