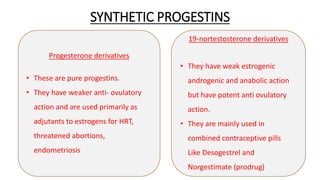
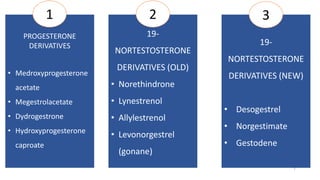
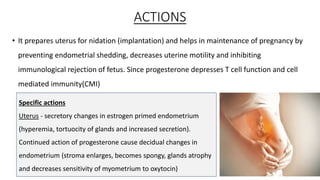
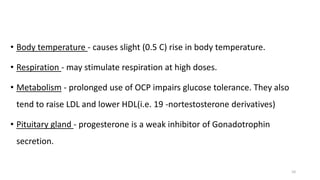
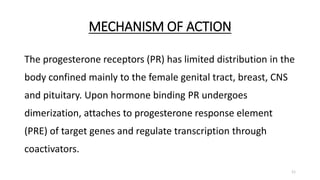
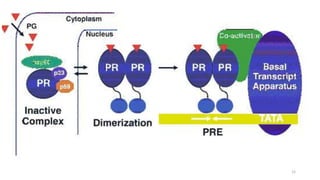
Progesterone is a natural hormone that prepares the uterus for pregnancy and helps maintain pregnancy. It can be produced naturally by the body or synthesized for medical uses. Progesterone has physiological actions in the uterus, cervix, vagina, breasts, central nervous system, and elsewhere to support pregnancy. It works by binding to progesterone receptors and regulating gene transcription. Progesterone and progestins are used for contraception, hormone replacement therapy, dysfunctional uterine bleeding, threatened miscarriage, endometriosis, and other conditions. Common side effects include changes in menstruation, headaches, and breast tenderness.
![• Males also produce 1-5mg progesterone per day from adrenals and
testes.
[BUT ROLE IN MALES IS NOT KNOWN]
5](https://image.slidesharecdn.com/progesteronereceptor-230726095318-71dcea5e/85/progesterone-receptor-pptx-5-320.jpg)