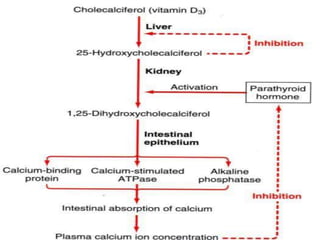
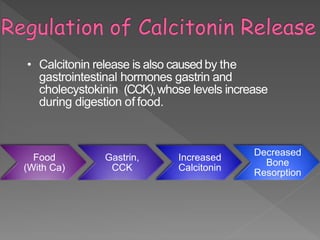
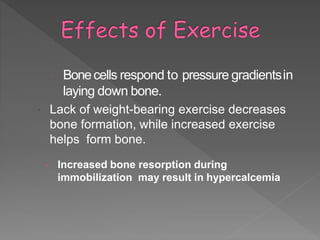
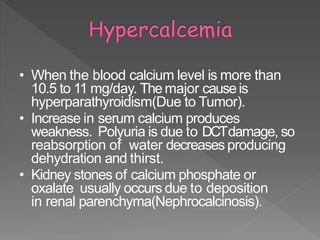
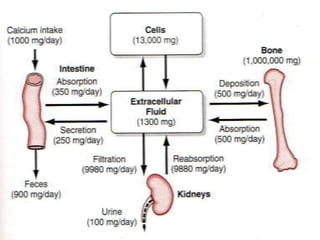
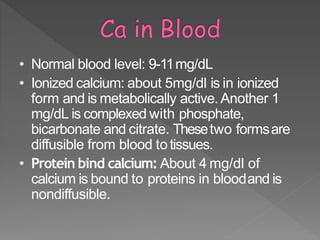
The document discusses the essential role of calcium in the human body, detailing its sources, absorption mechanisms, and physiological functions. It emphasizes the importance of adequate calcium intake to prevent conditions like osteoporosis, particularly highlighting hormonal regulation and the effects of various dietary components on calcium metabolism. Additionally, it outlines the consequences of calcium deficiency and the impact of lifestyle choices on bone health.









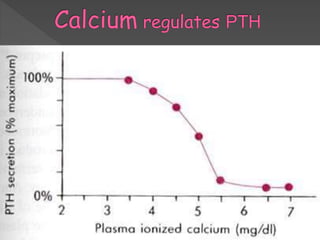
![• Thedominant regulator of PTHis plasma Ca2+.
• Secretion of PTHis inversely related to [Ca2+].
• Maximum secretion of PTHoccurs at plasma Ca2+below
3.5 mg/dL.
• At Ca2+above 5.5 mg/dL, PTHsecretion is maximally
inhibited.
• Aunique calcium receptor within the parathyroid cell
plasma membrane senseschangesin the extracellularfluid
concentration of Ca2+.
• Thisis atypical G-protein coupled receptor thatactivates
phospholipase Cand inhibits adenylate cyclase—result is
increase in intracellular Ca2+via generation of inositol
phosphates and decrease in cAMPwhich prevents
exocytosis of PTHfrom secretorygranules.](https://image.slidesharecdn.com/calcium-180326133957/85/Calcium-18-320.jpg)