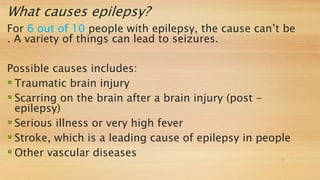
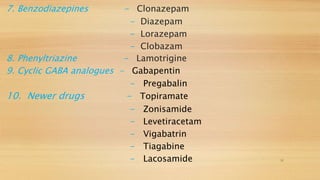
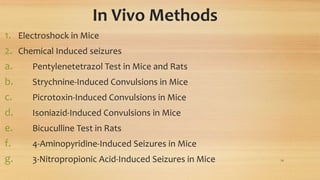
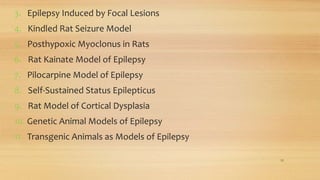
This document summarizes various in vitro and in vivo models used for anti-epileptic drug screening. The in vitro models described include tests measuring effects on GABA and glutamate receptors, transporters, and uptake/release. The in vivo models involve inducing seizures chemically or through focal lesions in rodents and examining effects of test compounds. Several genetic and transgenic animal models of epilepsy are also mentioned. The document provides details on procedures and evaluation methods for key screening tests involving GABA uptake/release in hippocampal slices and electroshock induction in mice.

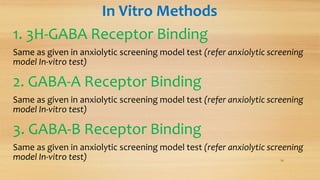
![In Vitro Methods
1. 3H-GABA Receptor Binding
2. GABA-A Receptor Binding
3. GABA-B Receptor Binding
4. 3H-GABA Uptake in Rat Cerebral Cortex Synaptosomes
5. GABA Uptake and Release in Rat Hippocampal Slices
6. Glutamate Receptors: [3H]CPP Binding
7. NMDA Receptor Complex: [3H]TCP Binding
8. Metabotropic Glutamate Receptors
9. Excitatory Amino Acid Transporters . . . . . . . . 13](https://image.slidesharecdn.com/antiepilepticscreeningmodel-190131055048/85/Anti-epileptic-screening-model-13-320.jpg)
![ Following two washes, slices (15mg) are incubated at 37°C for 15min in the
presence or absence of test compound.
[3H]-GABA is added and samples are incubated for an additional 5min
before filtration through Whatman GF/F filters.
Samples are then washed twice with 5ml ice-chilled 0.9% saline.
Distilled water is added and samples are allowed to sit at least 60min before
measured for radioactivity by liquid scintillation spectroscopy.
Blanks are treated in an identical manner but are left on ice throughoutthe
incubation.
18](https://image.slidesharecdn.com/antiepilepticscreeningmodel-190131055048/85/Anti-epileptic-screening-model-18-320.jpg)
![For measurement of GABA release, rat hippocampal slices are
prepared and dispersed in ice-cold HEPES buffered (pH7.2)
solution and incubated with 0.05µM [3H]-GABA for 15min at
Following two washes, the slices are incubated for an additional
finally resuspended in medium.
Tissue (10mg) is incubated at 37°C for a 15 min release period
presence or absence of test compound.
At the end of the release period, the medium is separated from
centrifugation at 500g for approximately 1 min and poured into
perchloric acid (0.4N).
The tissue is homogenized in 0.13 N perchloric acid.
Radioactivity in the samples is measured by using liquid
spectroscopy. 19](https://image.slidesharecdn.com/antiepilepticscreeningmodel-190131055048/85/Anti-epileptic-screening-model-19-320.jpg)