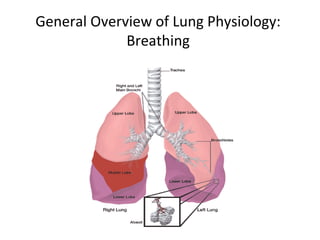
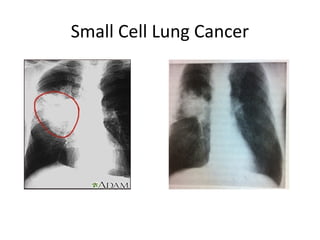
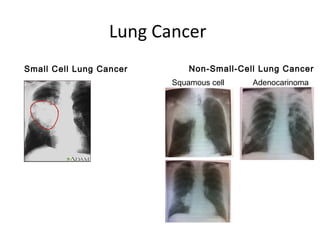
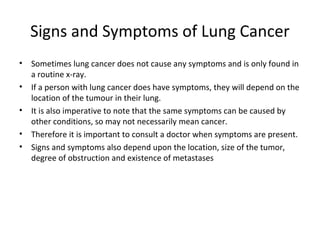
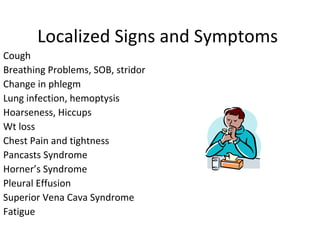
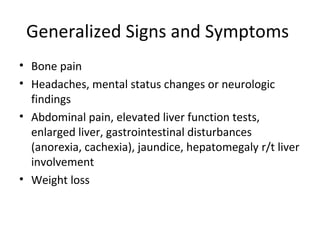
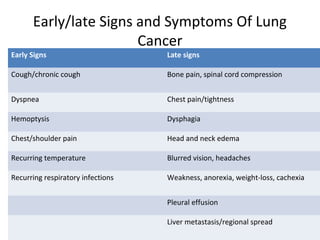
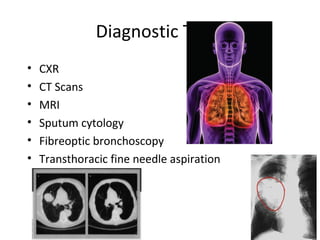
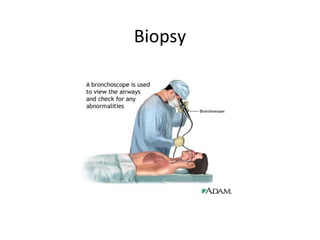
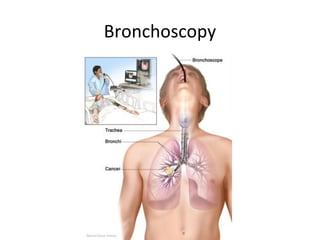
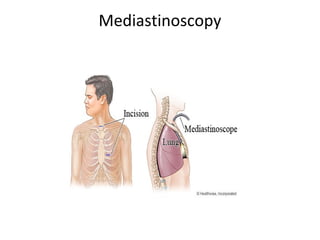
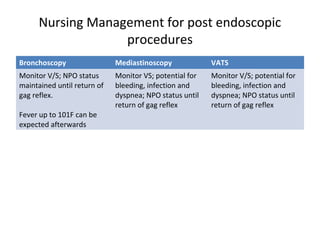
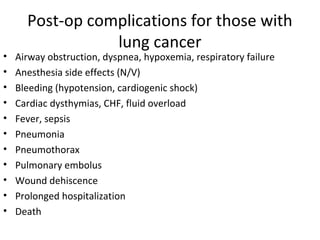
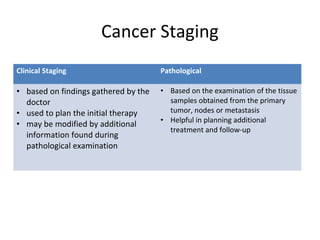
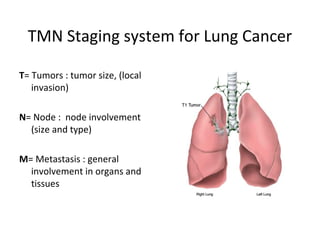
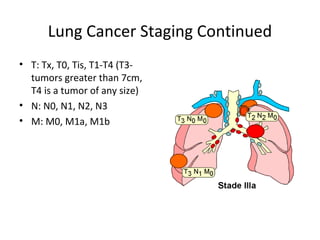
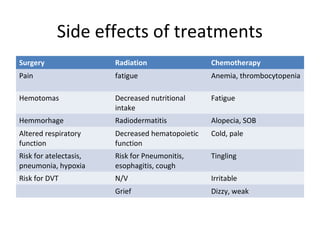
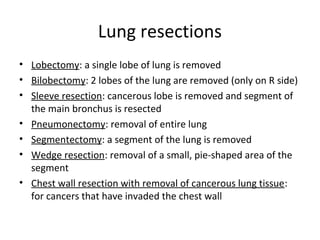
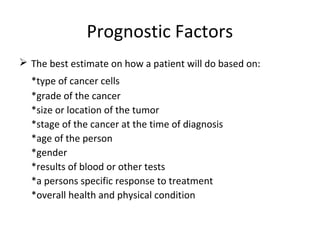
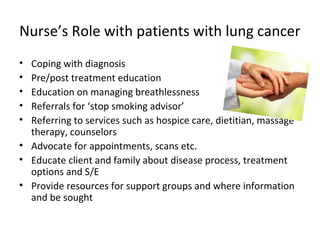
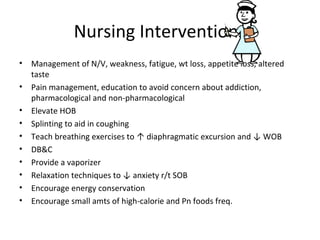
This document provides an overview of lung cancer, including the types, causes, risk factors, signs and symptoms, diagnostic tests, staging, treatments, side effects, and nursing management. It discusses the two main types of lung cancer - small cell lung cancer and non-small cell lung cancer (NSCLC). NSCLC makes up about 80% of cases and includes squamous cell carcinoma, adenocarcinoma, and large cell carcinomas. Risk factors include smoking and environmental exposures. Signs and symptoms depend on the location and size of the tumor. Diagnostic tests include imaging, biopsies, and lab tests. The TNM system is used for staging. Treatments include surgery, radiation, chemotherapy, with side effects like