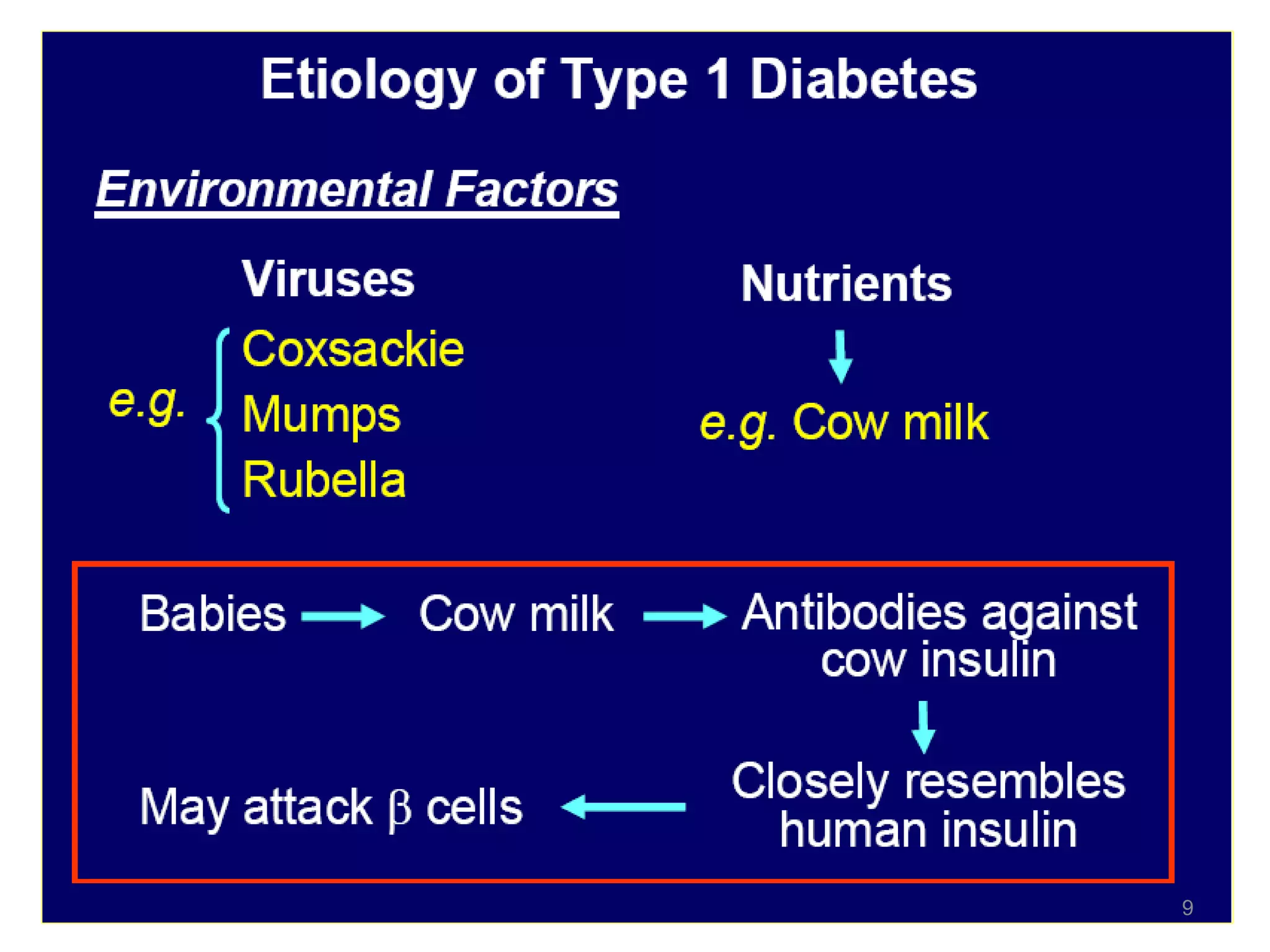
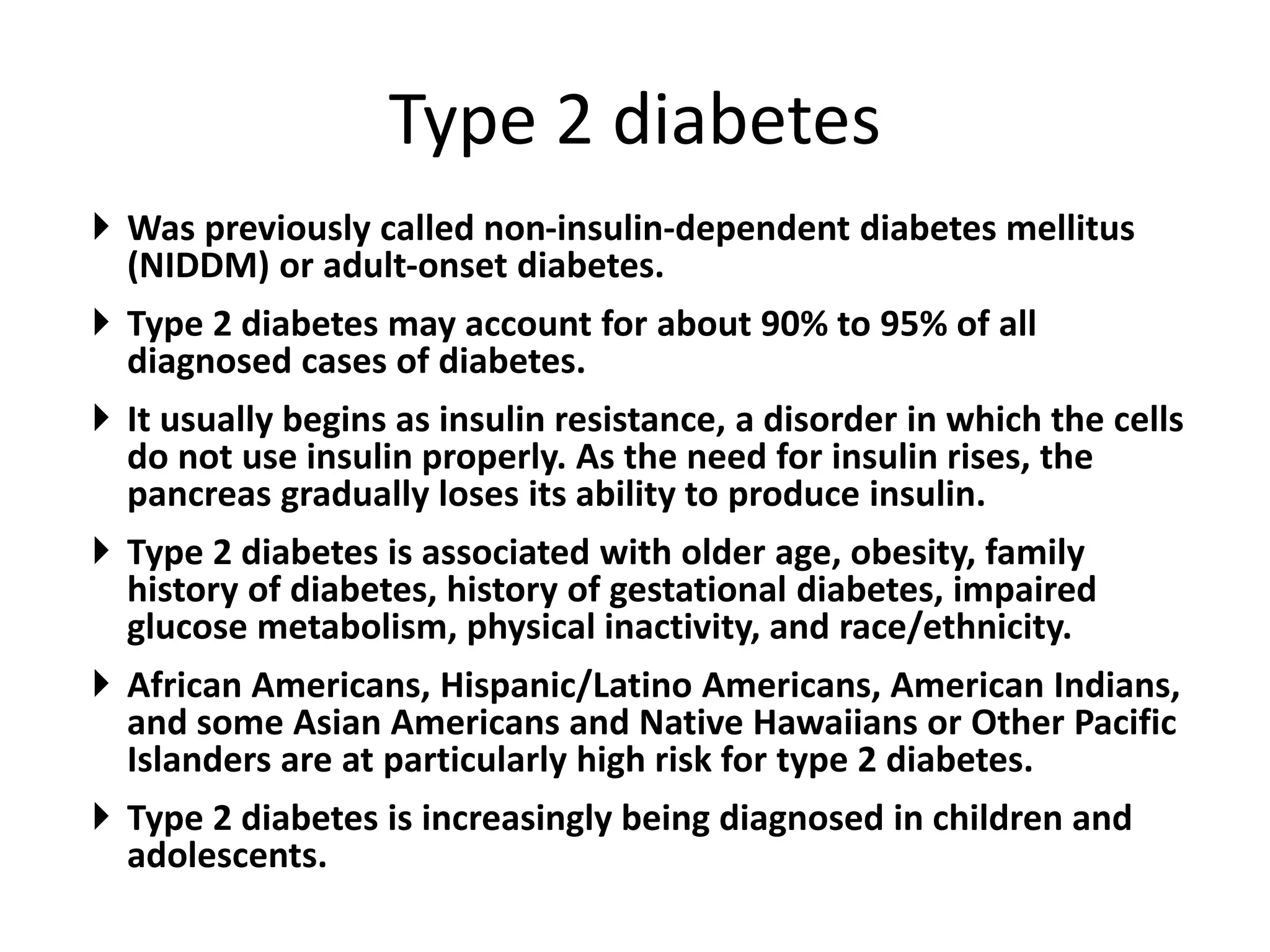
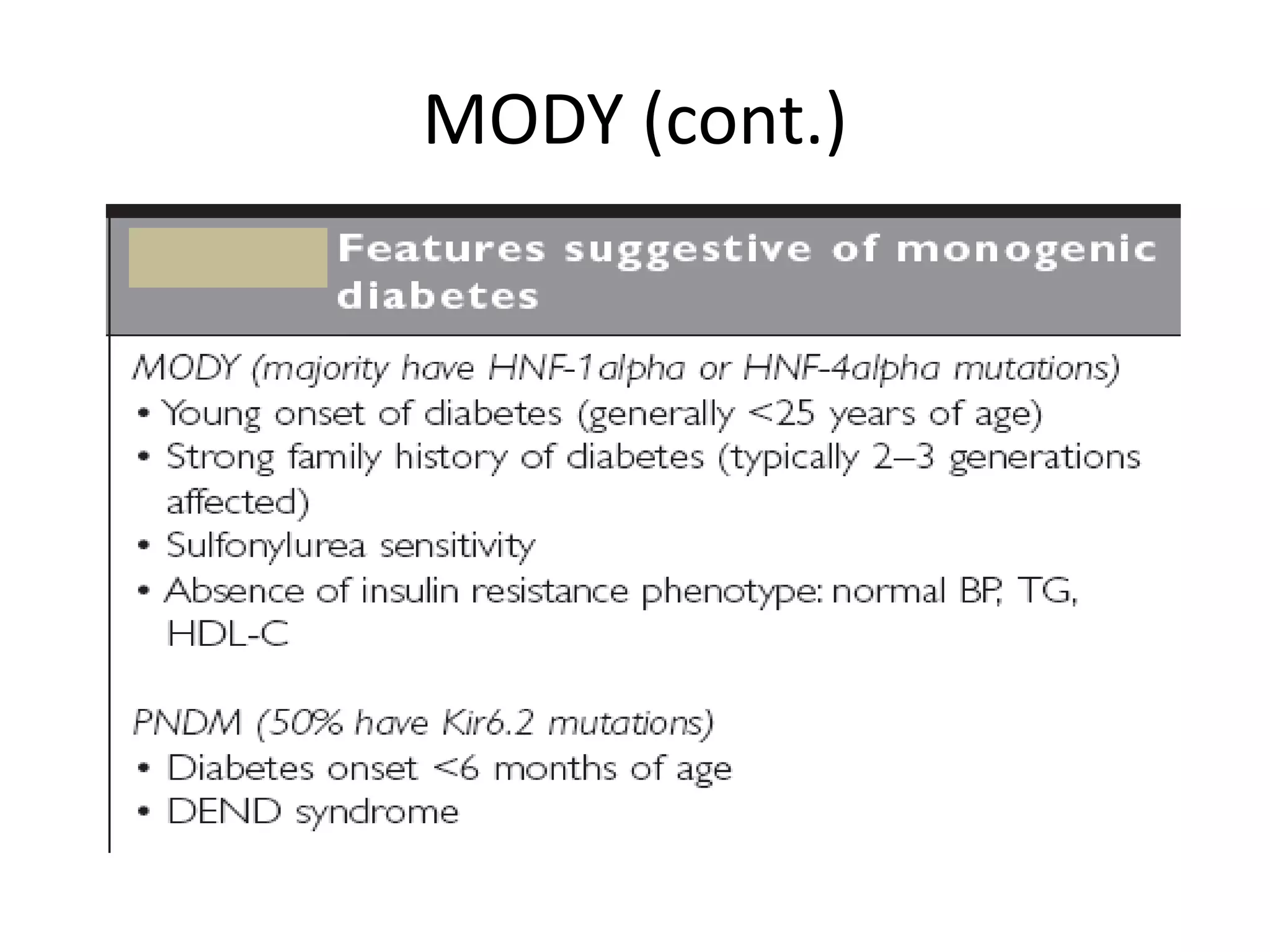
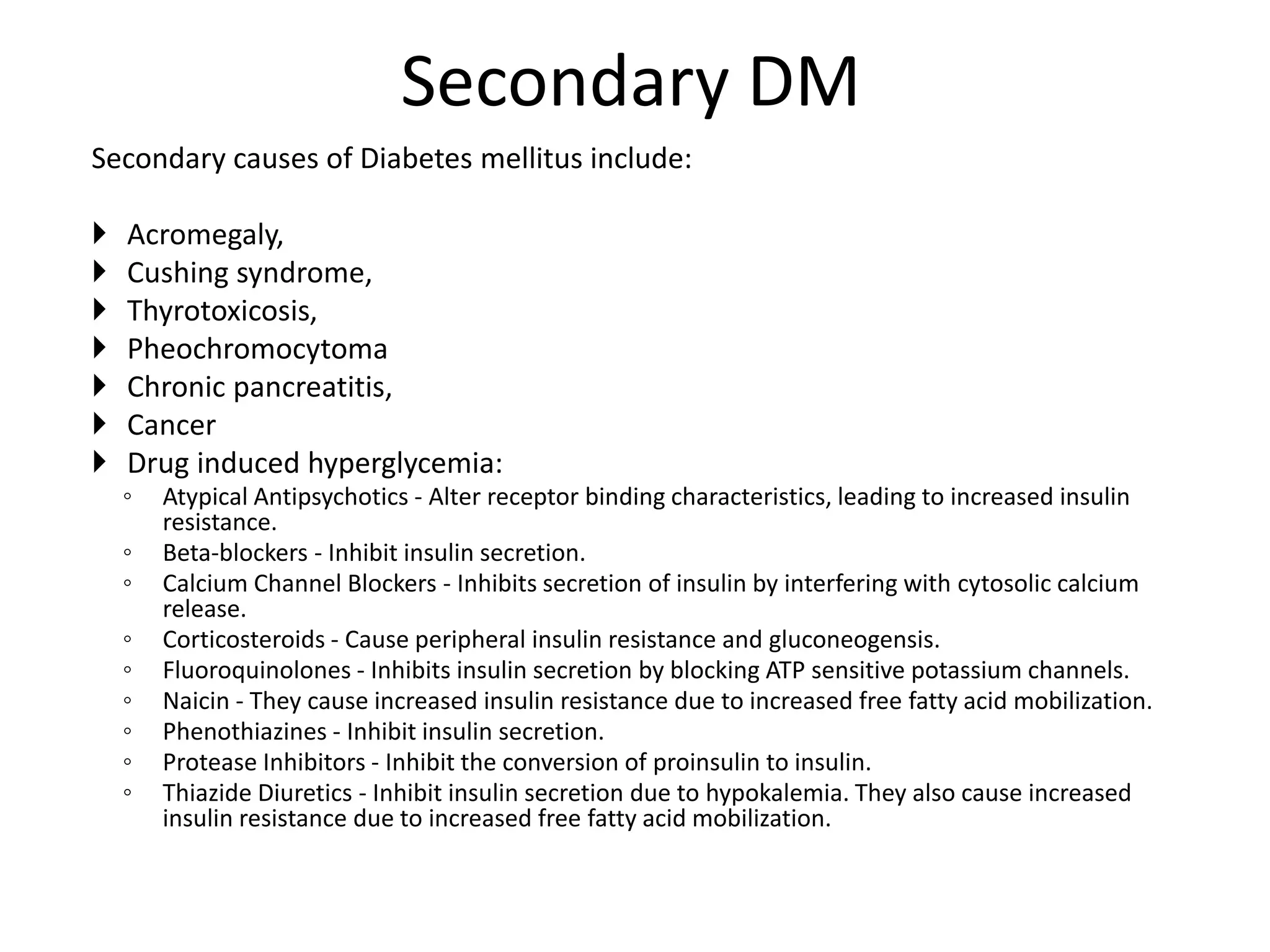
The document discusses diabetes mellitus (DM), which is characterized by high blood glucose levels due to defects in insulin production or action. There are two main types of DM: Type 1 is an autoimmune disease where the body destroys insulin-producing cells, while Type 2 is associated with obesity and aging and results from insulin resistance and relative insulin deficiency. Gestational diabetes occurs during pregnancy and increases risk of future Type 2 DM. Other types include genetic disorders. The prevalence of DM, especially Type 2, is increasing worldwide due to rising obesity and physical inactivity.