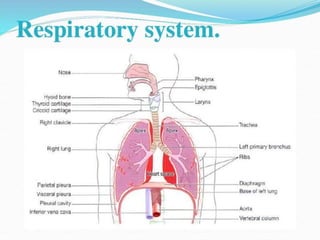
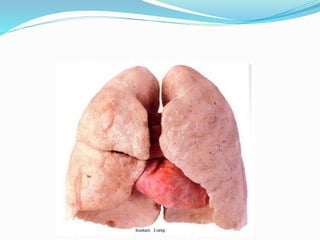
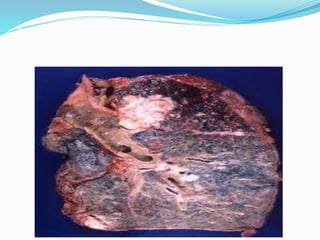
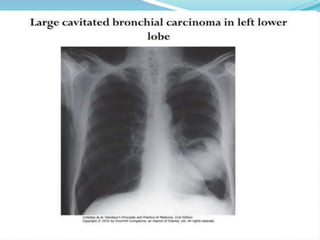
This document provides an outline and overview of lung cancer (bronchial carcinoma). It discusses the epidemiology, risk factors like smoking, pathogenesis, types, staging systems, clinical features, diagnosis, management including surgery and chemotherapy, complications, differential diagnosis, prognosis and conclusions. The respiratory system, normal physiology, and common radiological presentations are also outlined.