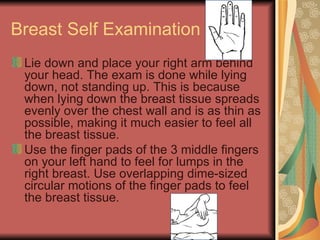
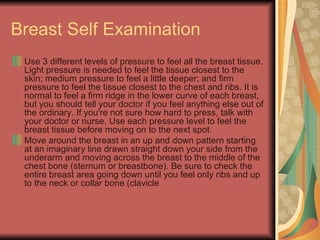
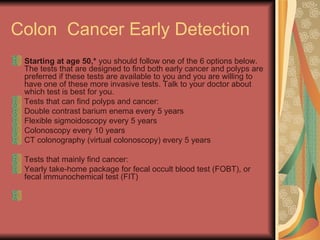
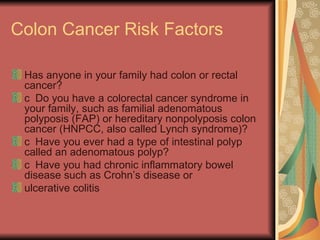
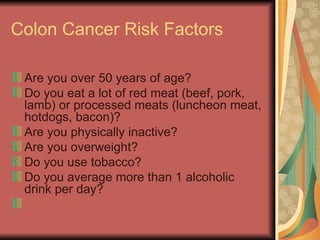
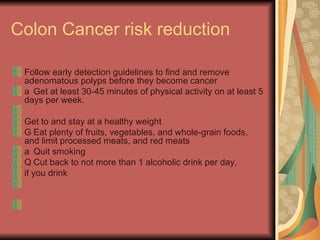
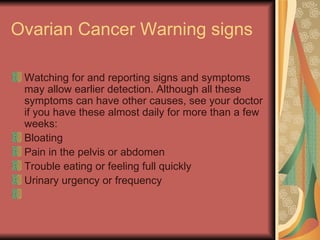
The document provides information about various cancers including warning signs, risk factors, screening guidelines, and Medicare coverage. For breast cancer, it discusses self-examination techniques and recommends yearly mammograms starting at age 40. For lung cancer, it states the main risk factor is smoking and there are no recommended screening tests. Colon cancer screening is recommended starting at age 50 using various tests. Medicare covers some screening and counseling services.