This document provides an overview of lung cancer, including:
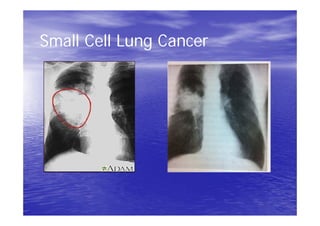
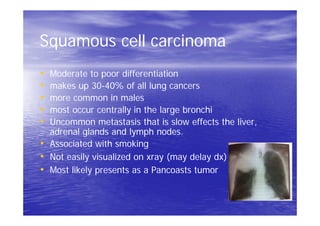
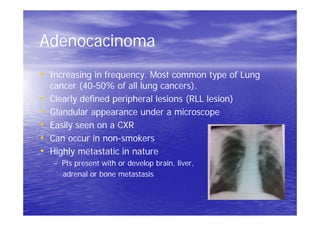
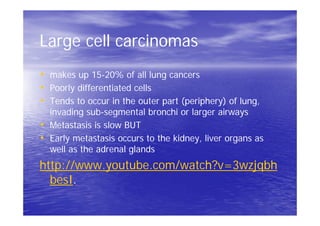
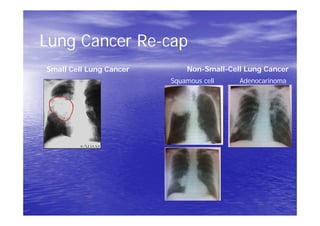
1) It describes the two main types of lung cancer - small cell lung cancer and non-small cell lung cancer - and the most common subtypes.
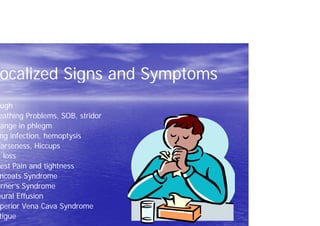
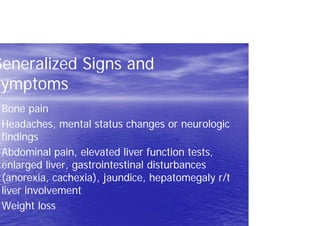
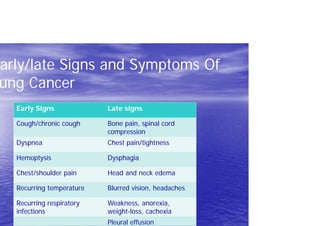
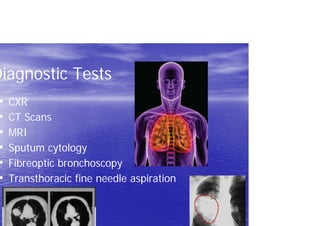
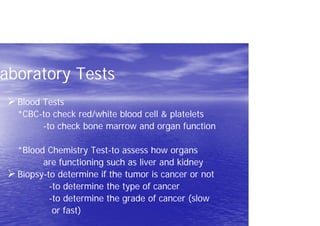
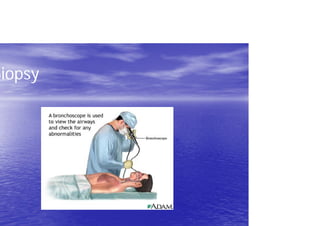
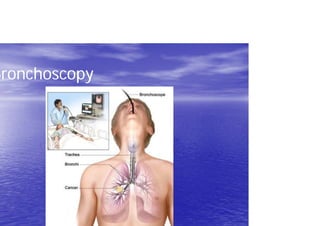
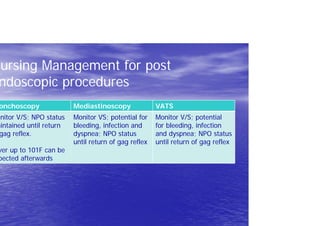
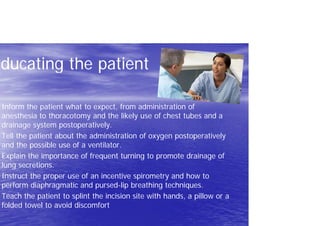
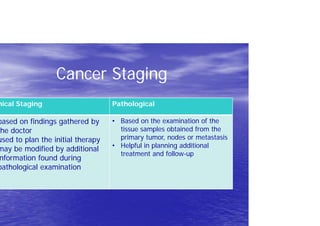
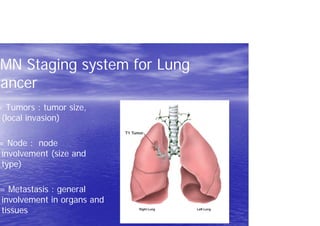
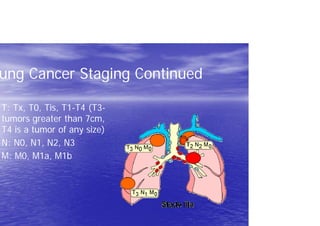
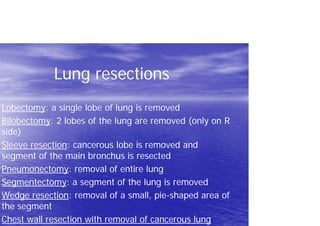
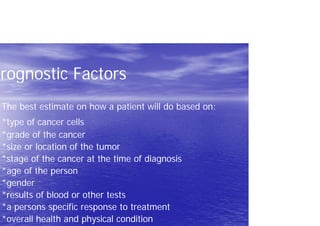
2) Risk factors, signs and symptoms, diagnostic tests, staging, and treatments are discussed.
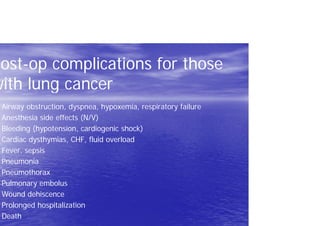
3) Post-op complications can include issues like respiratory failure, bleeding, and infection that nurses must monitor for.