This document discusses several types of blistering diseases:
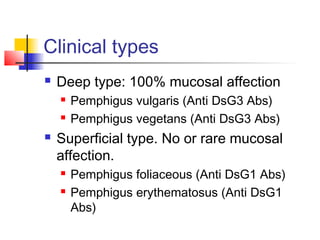
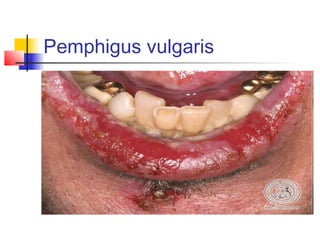
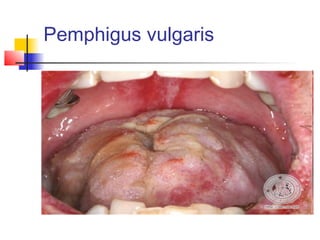
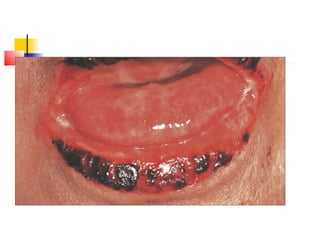
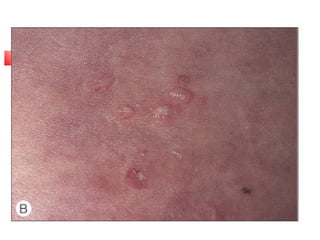
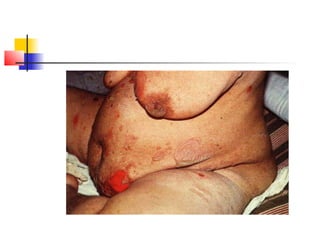
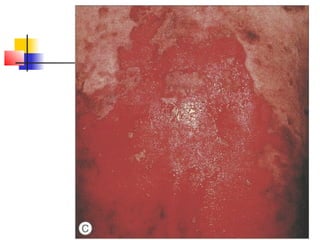
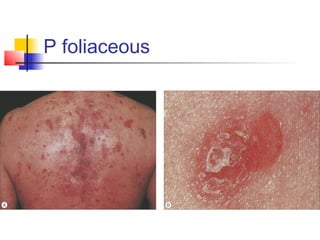
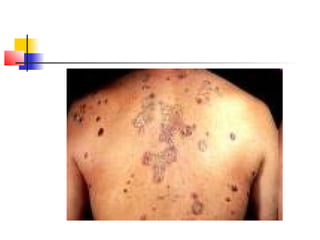
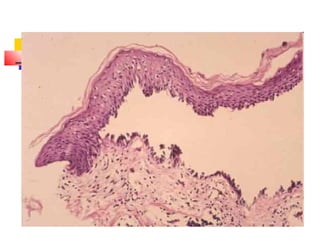
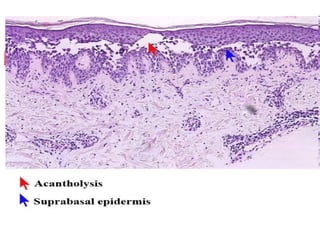
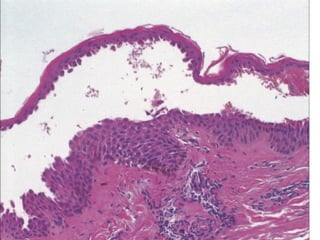
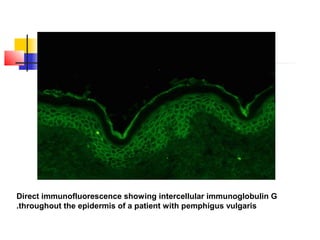
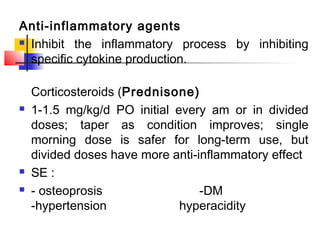
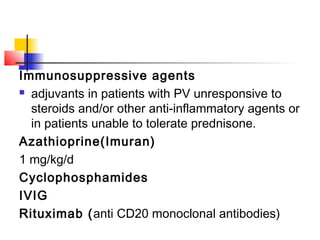
1. Pemphigus is an autoimmune blistering disease caused by antibodies against desmoglein proteins, resulting in loss of cell adhesion between keratinocytes. Pemphigus vulgaris primarily affects the mucosa and has a mortality rate of 5-15%.
2. Dermatitis herpetiformis is associated with celiac disease and gluten sensitivity. It is characterized by grouped blisters and erosions on the elbows and knees. Treatment involves a gluten-free diet and dapsone.
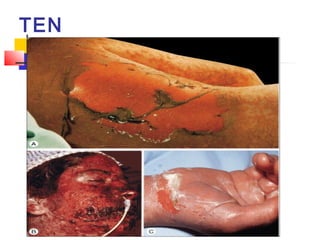
3. Staphylococcal scalded skin syndrome and toxic epidermal necrolysis are severe blistering