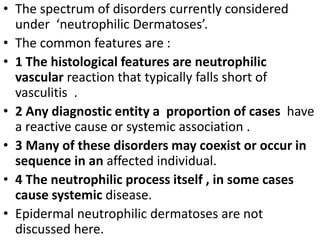
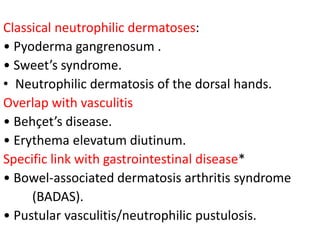
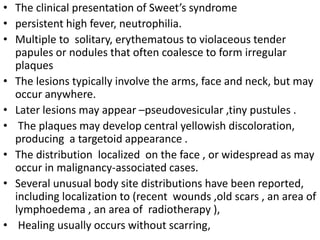
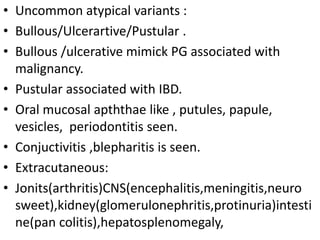
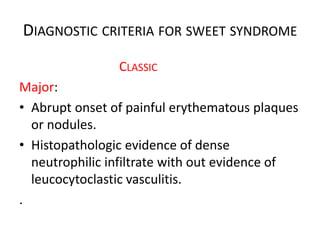
This document discusses neutrophilic dermatoses, a spectrum of disorders characterized by neutrophilic infiltration of the skin without true vasculitis. Key points include:
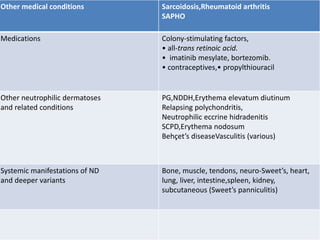
- Common features include a neutrophilic vascular reaction, some cases having a reactive or systemic cause, disorders may coexist or occur sequentially in individuals.
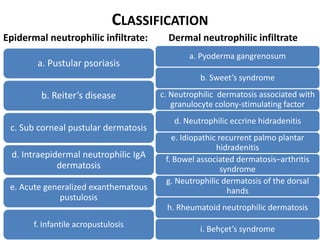
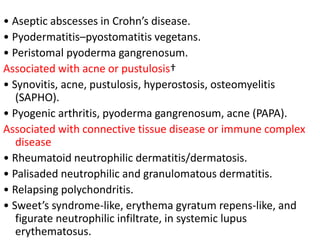
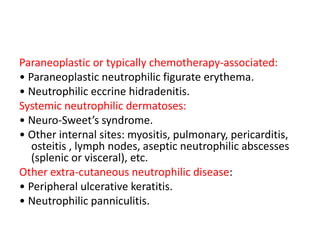
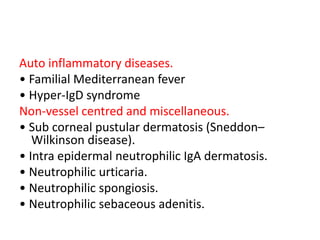
- Classification includes disorders grouped by location of neutrophilic infiltrate (epidermal vs dermal).
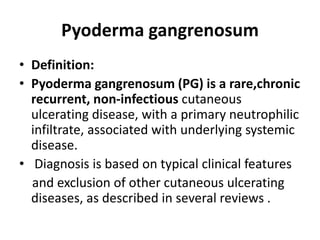
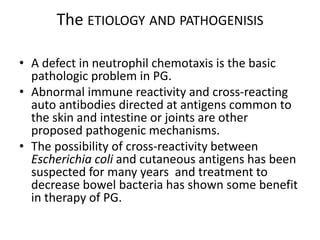
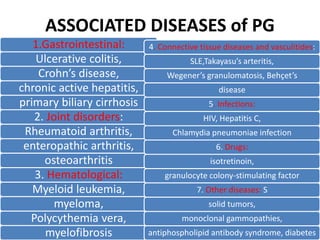
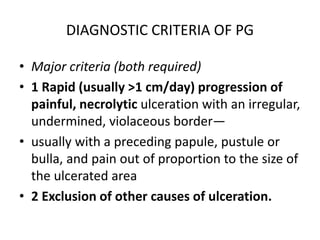
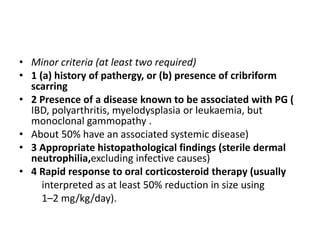
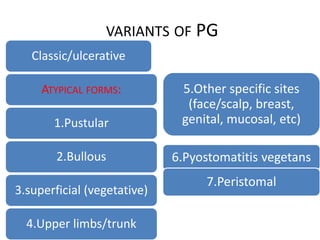
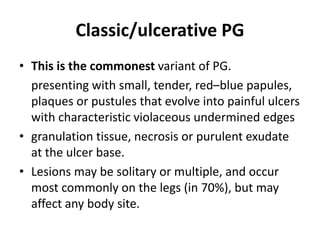
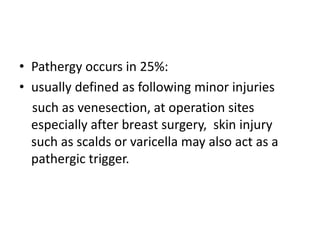
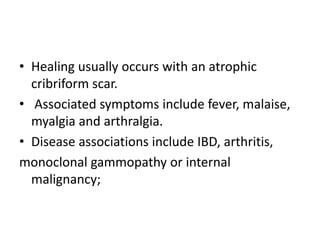
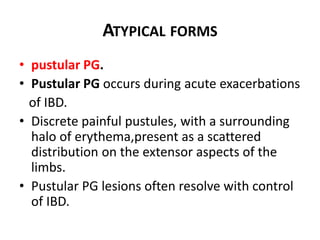
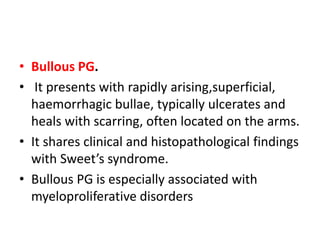
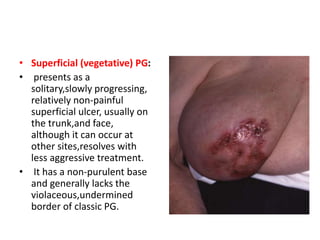
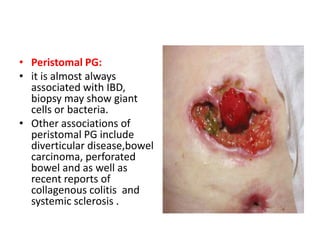
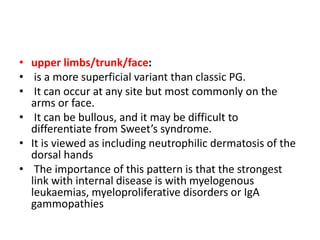
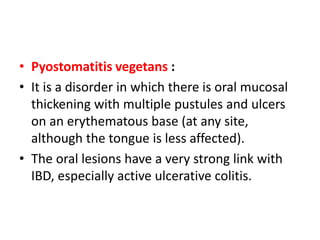
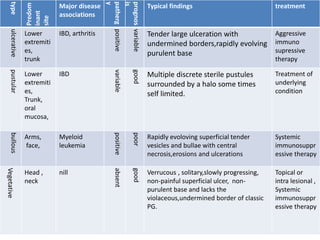
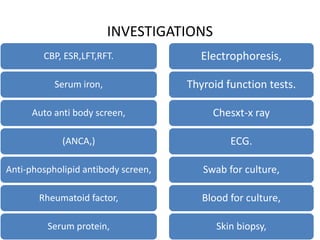
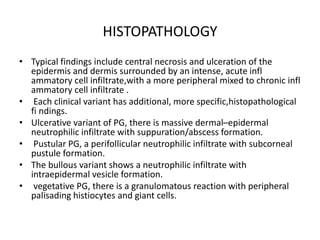
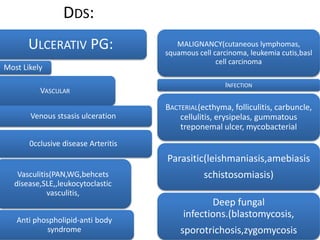
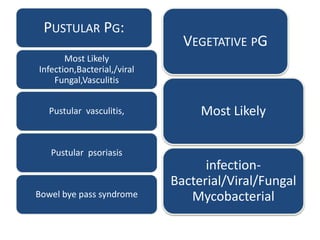
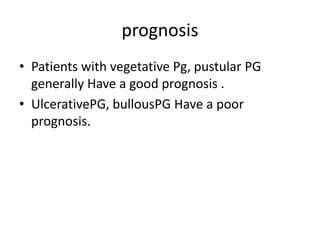
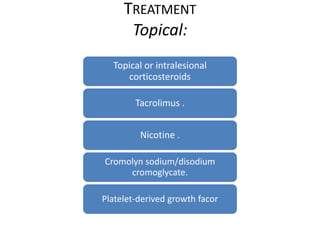
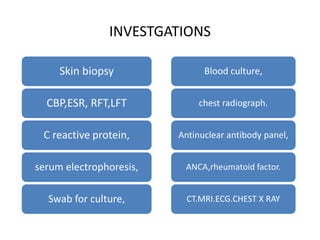
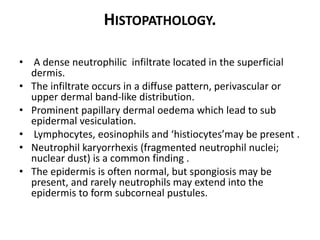
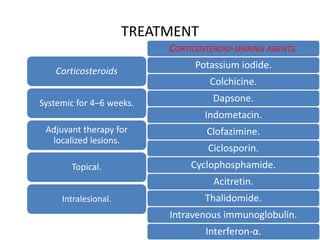
- Pyoderma gangrenosum is discussed in depth, including its pathogenesis, associated diseases, diagnostic criteria, variants (classic, pustular, bullous etc.), investigations and histopathology. Treatment involves immunosuppressive therapy.