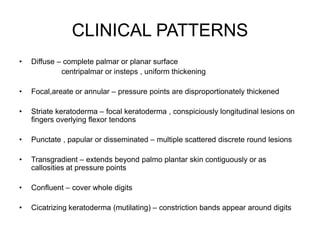
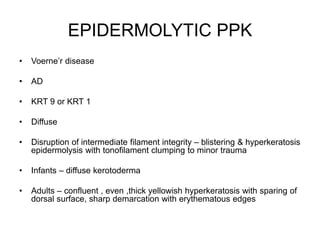
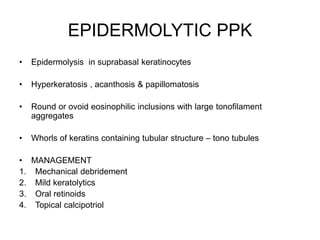
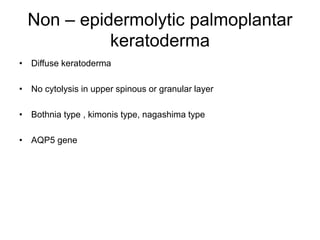
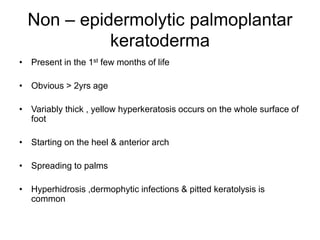
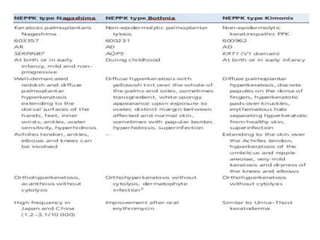
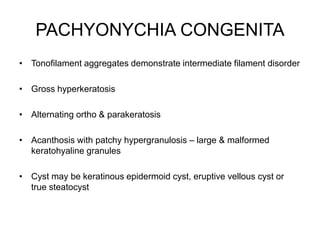
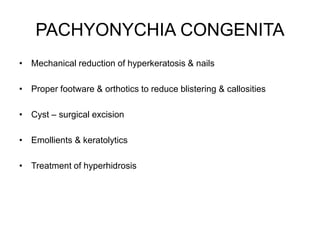
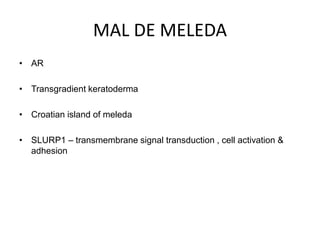
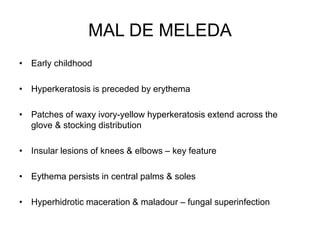
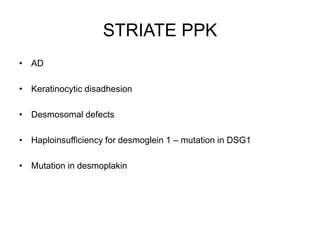
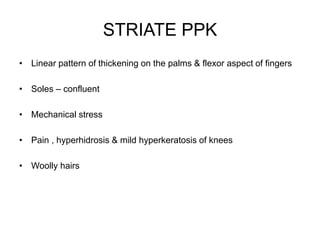
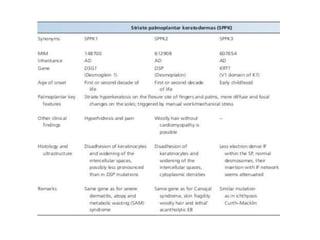
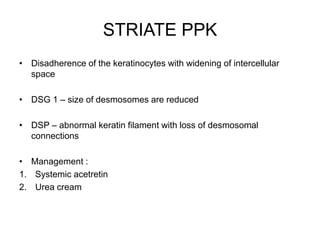
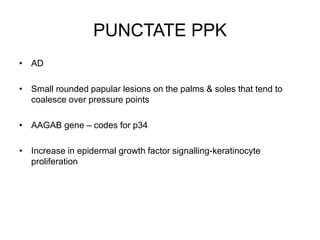
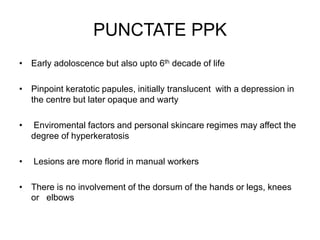
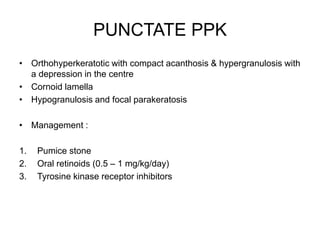
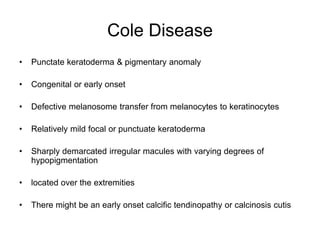
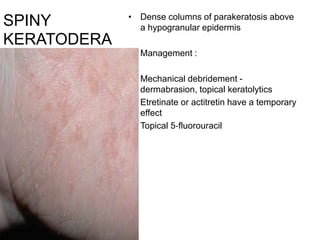
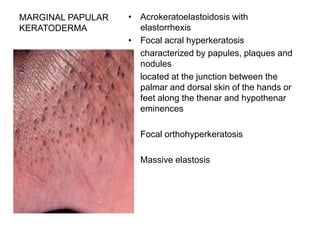
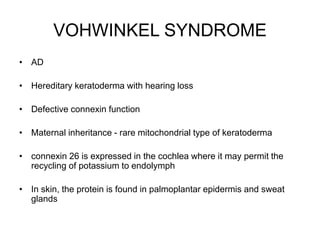
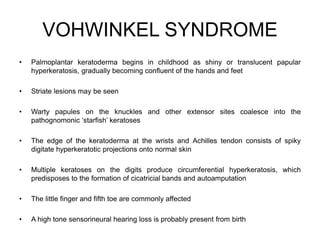
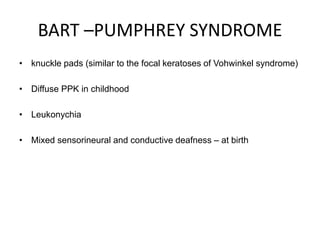
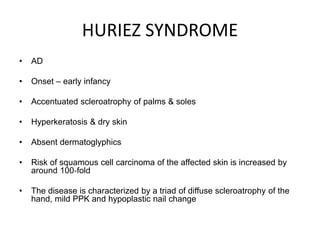
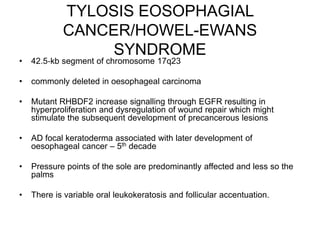
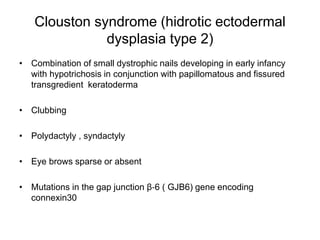
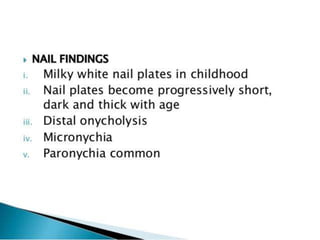
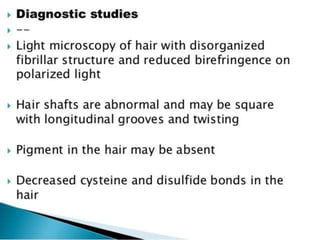
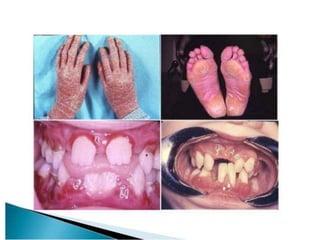
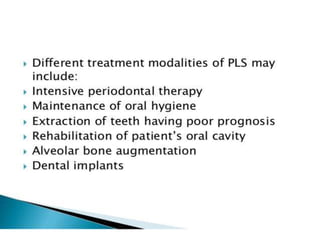
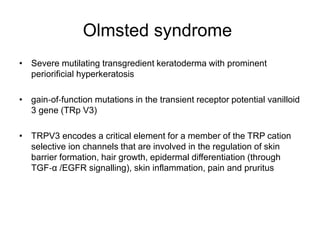
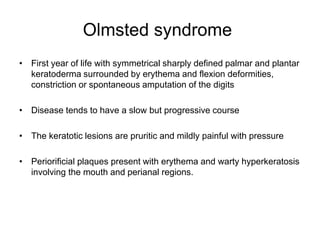
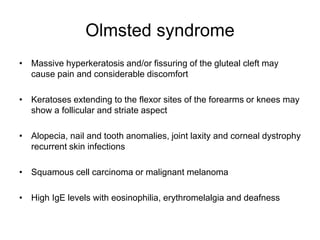
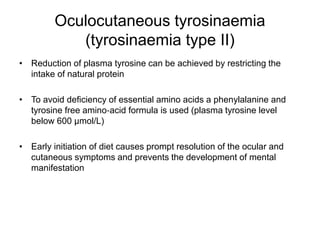
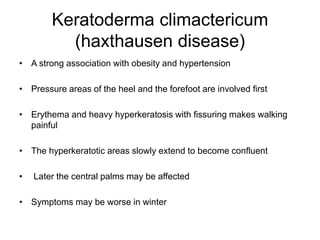
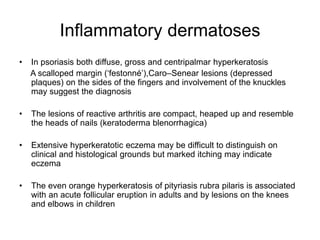
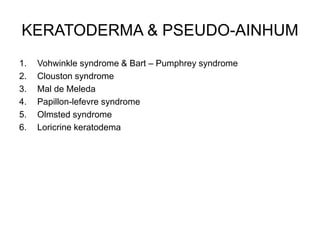
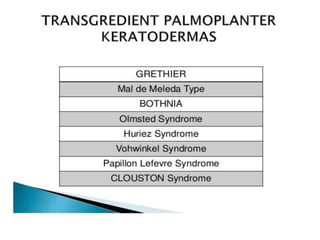
This document provides information on various types of palmoplantar keratoderma (PPK). It describes the clinical patterns, genetic causes, histopathological findings, and management options for different syndromic and non-syndromic forms of PPK, including epidermolytic, punctate, striate, and transgradient PPK as well as disorders associated with PPK like pachyonychia congenita and Naxos syndrome. The document discusses the characteristic features, genetic defects, and treatment approaches for these PPK subtypes.