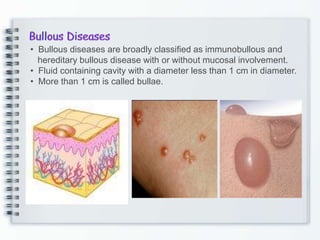
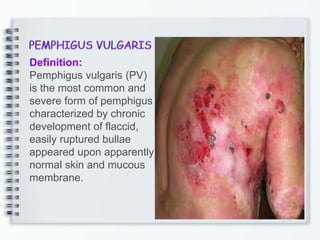
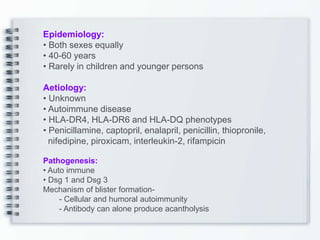
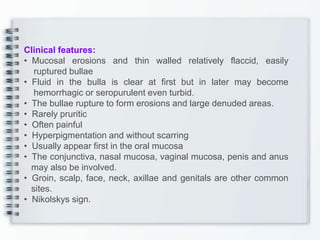
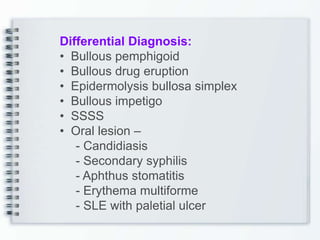
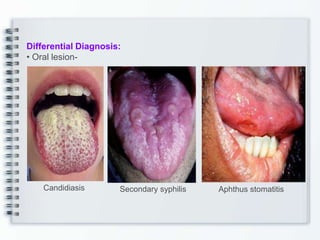
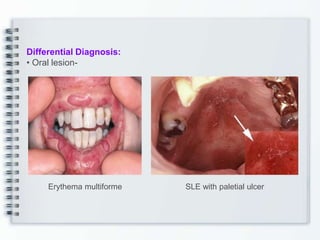
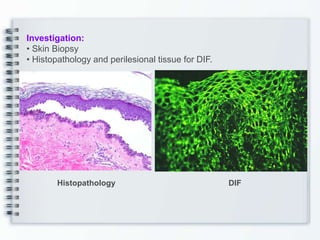
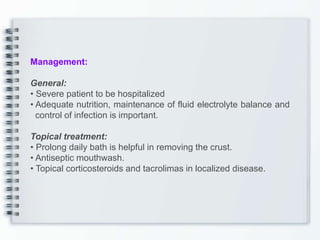
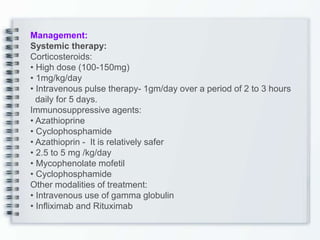
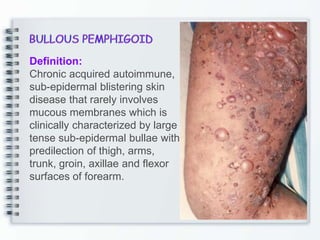
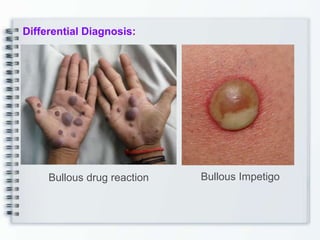
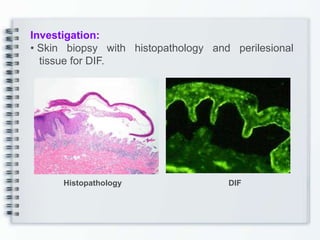
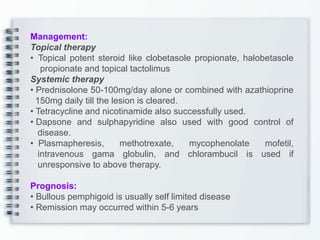
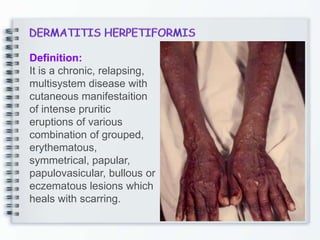
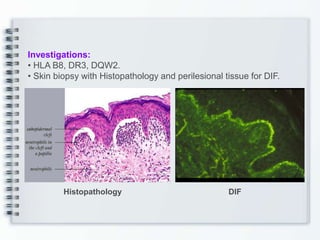
This document discusses several bullous diseases including pemphigus vulgaris, bullous pemphigoid, and dermatitis herpetiformis. It provides definitions, epidemiology, clinical features, investigations including histopathology and direct immunofluorescence findings, differential diagnoses, and management strategies for each condition. Key points include that pemphigus vulgaris is an autoimmune disease causing flaccid bullae on skin and mucous membranes, bullous pemphigoid features large tense subepidermal bullae mainly on the trunk and limbs, and dermatitis herpetiformis causes pruritic papular and bullous lesions that heal with scarring.