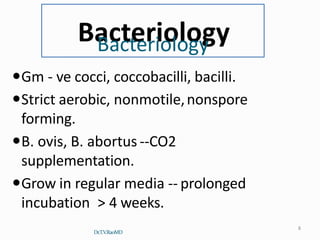
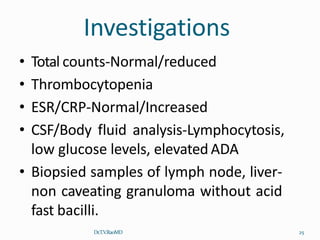
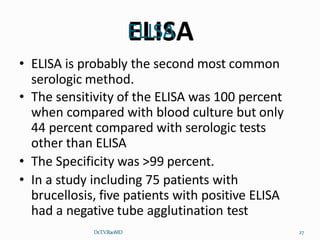
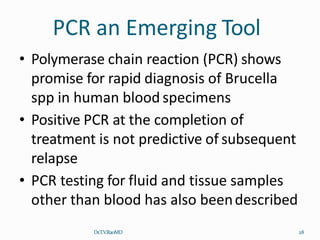
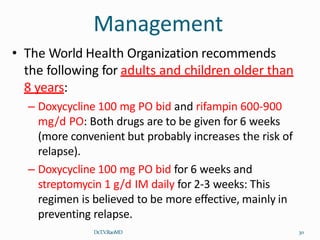
Brucellosis is a zoonotic bacterial infection caused by ingesting unpasteurized dairy products or having direct contact with infected animal fluids from livestock such as cattle, goats, and pigs. It causes non-specific flu-like symptoms such as fever, night sweats, joint pain, and fatigue. Diagnosis involves serological tests to detect antibodies and PCR to detect the bacteria. Treatment consists of a combination antibiotic regimen for 6 weeks such as doxycycline plus streptomycin or doxycycline plus rifampin to reduce the risk of relapse.