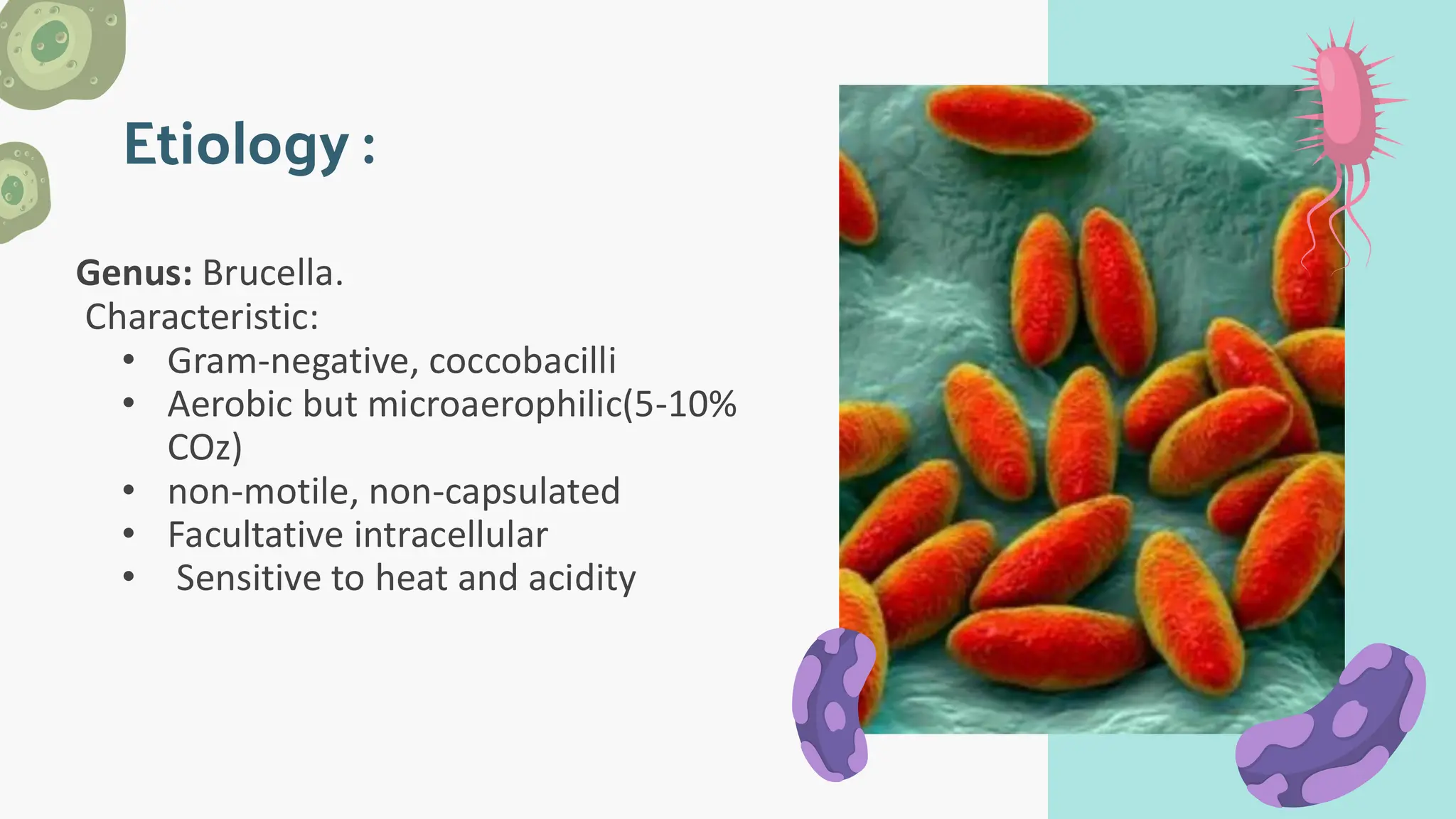
Brucellosis is a zoonotic infectious disease caused by Brucella bacteria, with symptoms ranging from fever and headache in the acute phase to chronic issues like arthritis and endocarditis if untreated. It is predominantly transmitted through direct contact with infected animals or consumption of unpasteurized dairy, with annual cases reaching 500,000 globally, especially in endemic regions. Diagnosis involves serologic tests and blood cultures, while treatment typically includes antibiotics like doxycycline and rifampicin; prevention strategies focus on vaccination in animals and public awareness.