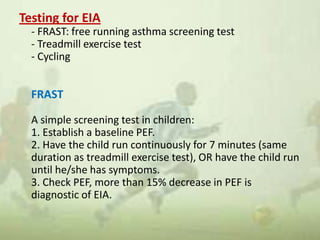
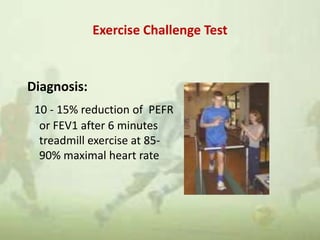
Exercise-induced asthma (EIA) and bronchospasm are triggered by exercise in patients with or without chronic asthma. EIA is diagnosed when exercise causes a 15% decrease in lung function and symptoms start after exercise and resolve within 60 minutes. It is common, affecting 10-20% of the general population and up to 90% of asthmatics. Treatment includes warm-up/cool-down periods, medication before exercise like bronchodilators, and ensuring proper asthma management.