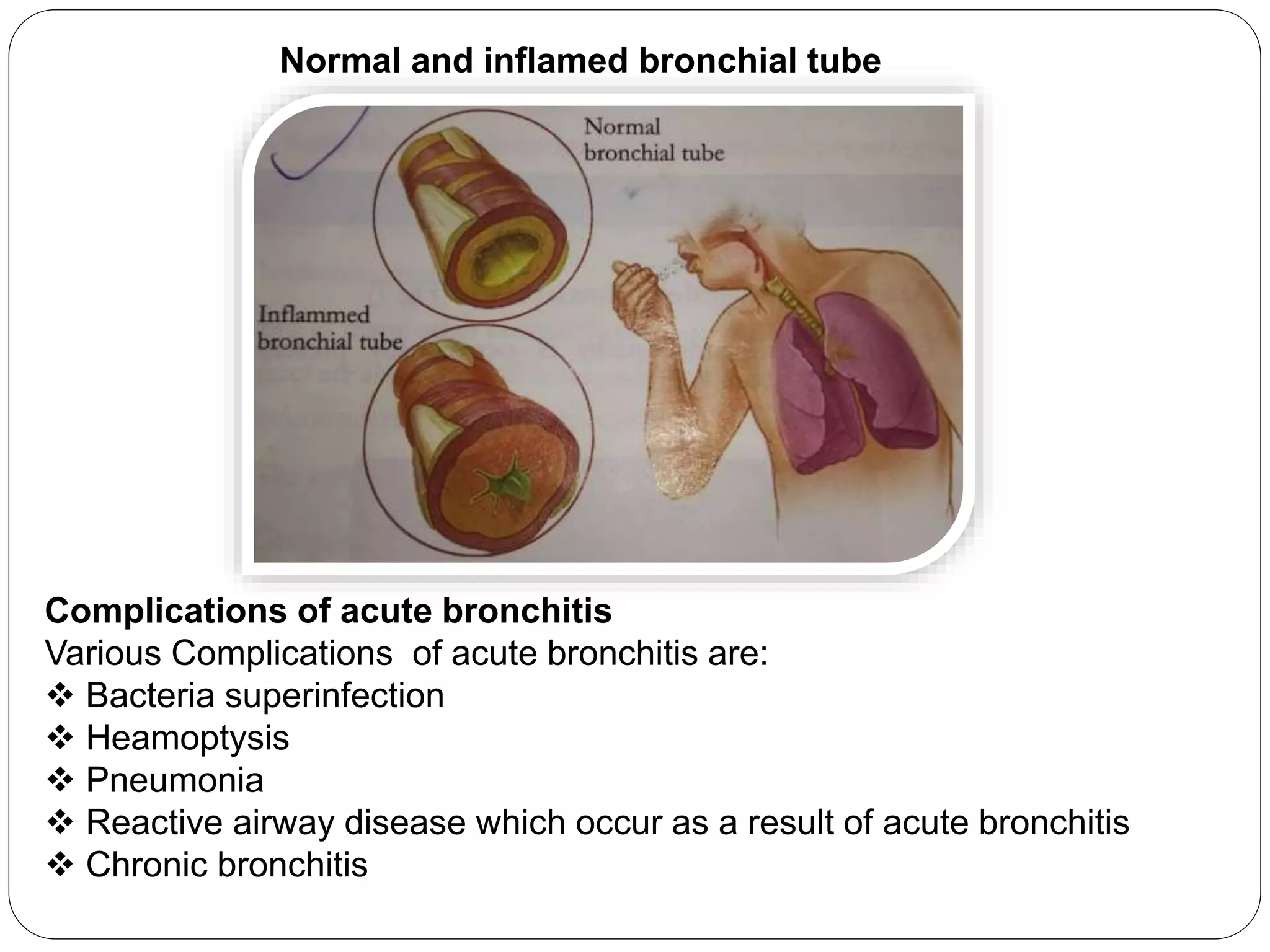
This document summarizes a presentation on acute and chronic bronchitis. It begins by defining acute bronchitis as inflammation of the large bronchi caused by bacterial or viral infection. It then compares acute and chronic bronchitis, noting their differences in pathogens, onset, duration, age groups affected, and clinical presentation. The document discusses the epidemiology and risk factors of acute bronchitis. It covers the infectious and non-infectious causes, pathophysiology, clinical presentation, diagnosis, treatment including pharmacological and non-pharmacological approaches, patient education, and prognosis. The presentation aims to provide an overview of acute and chronic bronchitis for healthcare professionals.