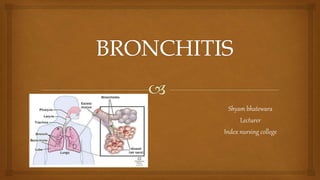
Bronchitis is an inflammation of the bronchial tubes that carry air to and from the lungs. It is commonly caused by viral infections like colds or flu, but can also be bacterial. Symptoms include cough, fever, shortness of breath, and wheezing. Diagnosis is made through physical exam and listening to the lungs. Treatment focuses on relieving symptoms, using medications like antibiotics (for bacterial cases), bronchodilators, cough suppressants, and ensuring proper hydration. Patients are educated on medication use, seeking medical care if symptoms worsen, using humidifiers, and doing deep breathing exercises.