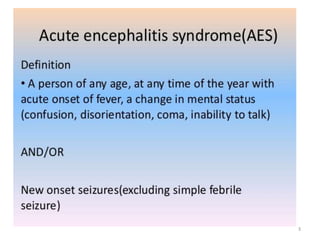
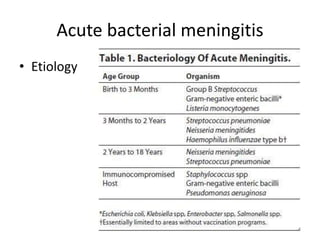
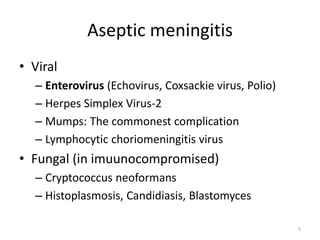
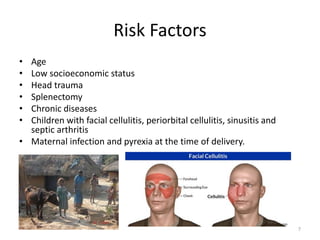
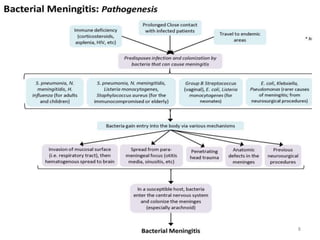
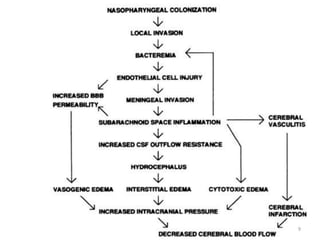
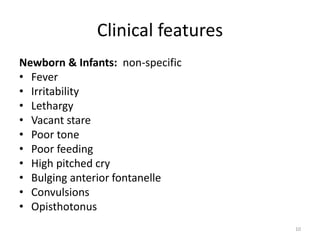
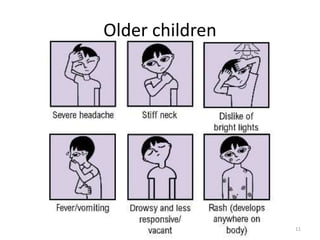
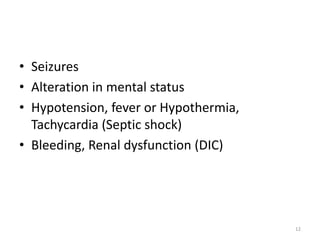
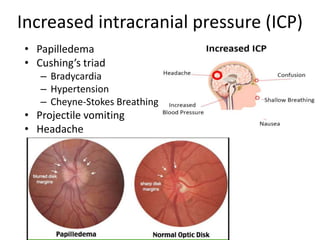
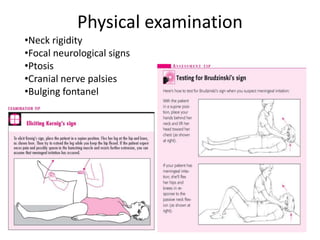
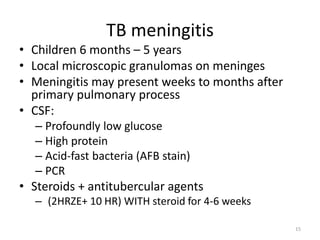
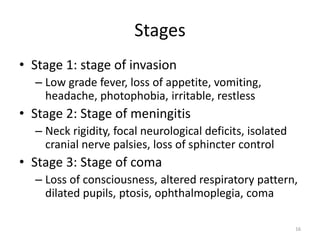
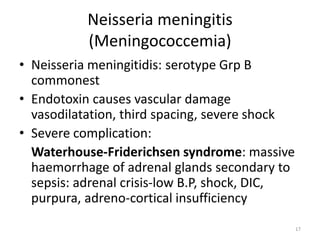
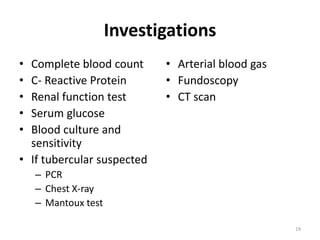
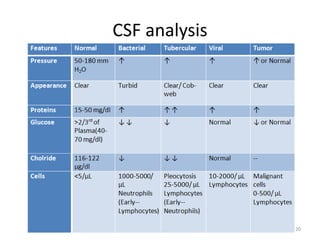
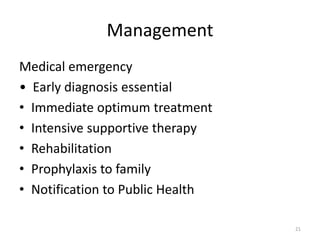
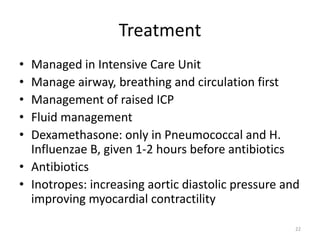
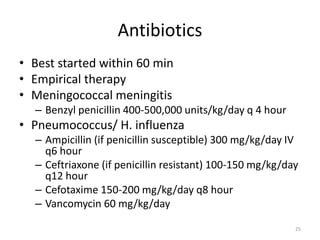
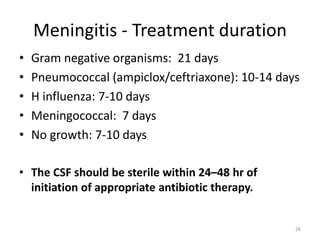
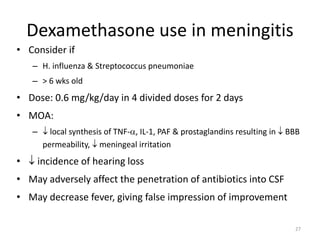
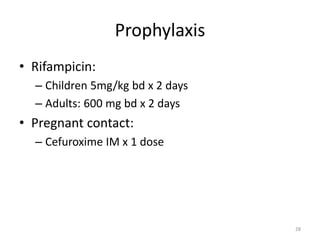
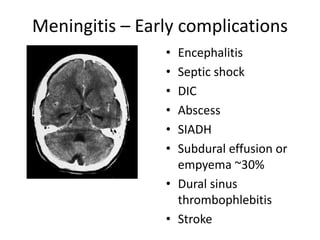
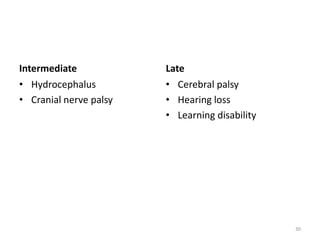
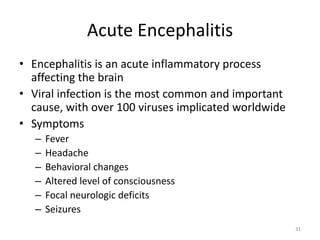
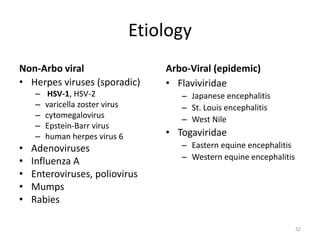
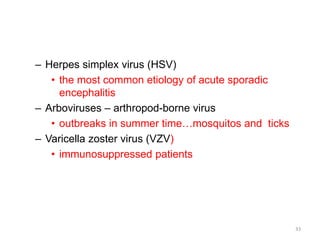
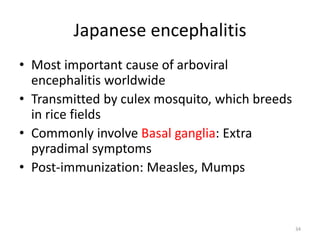
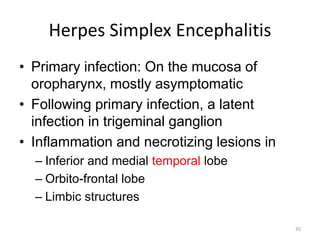
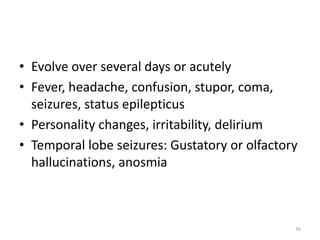
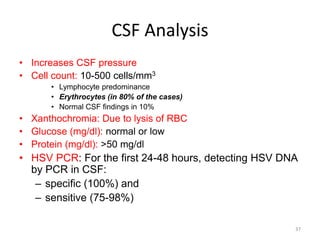
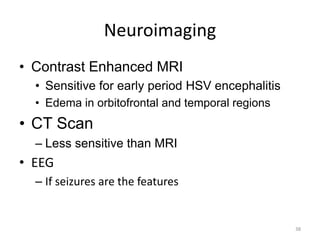
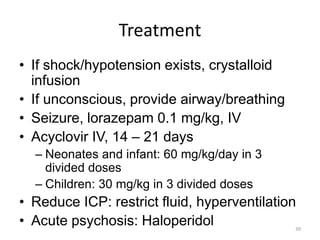
The document provides a comprehensive overview of acute meningoencephalitis, detailing its definition, causes, risk factors, clinical features, and management approaches. It covers bacterial and viral causes, including specific conditions like tuberculosis meningitis and various complications such as septic shock and encephalitis. Therapeutic strategies include the need for early diagnosis, intensive supportive care, and appropriate antibiotic treatment based on the causative organism.