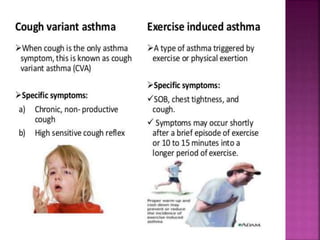
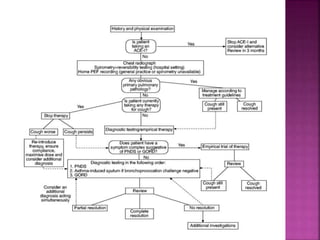
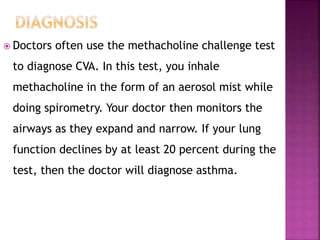
Chronic cough, notably cough-variant asthma (CVA), is frequently encountered in primary care, characterized primarily by a dry cough without typical asthma symptoms. Diagnosis often relies on the efficacy of bronchodilator therapy and may require the methacholine challenge test for confirmation. Treatment typically includes inhaled corticosteroids, oral medications, and bronchodilators, with referral to specialists for persistent cases.