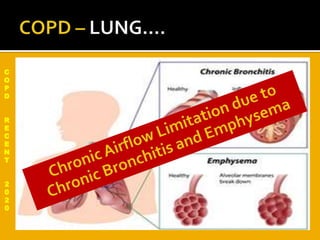
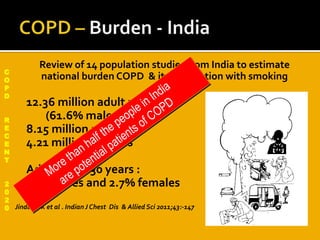
The document reviews several studies on chronic obstructive pulmonary disease (COPD) in India and clinical trials of various COPD medications:
- An estimated 12.36 million Indian adults have COPD, with higher prevalence in males (5%) than females (2.7%).
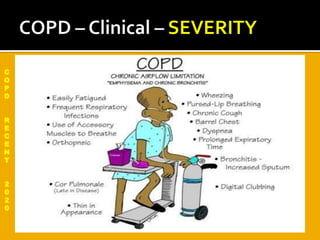
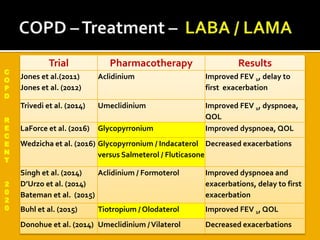
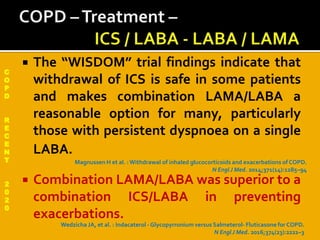
- Recent trials show new long-acting bronchodilators like umeclidinium and glycopyrronium improve lung function, dyspnea, and quality of life in COPD. Combinations of long-acting beta-agonists (LABAs) and long-acting muscarinic antagonists (LAMAs) provide benefits over monotherapies.
- Studies provide evidence for the use of LAMAs in