This document provides information on breast swelling including:
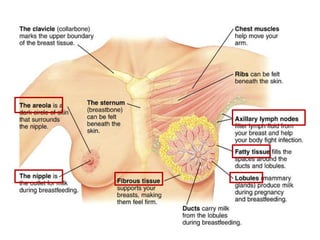
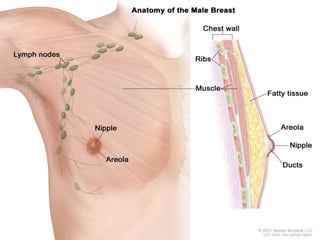
- Definitions of breast swelling and a short anatomy of the breast.
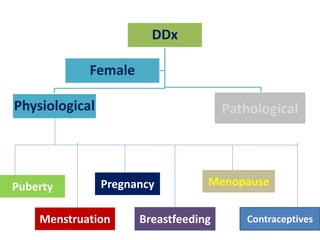
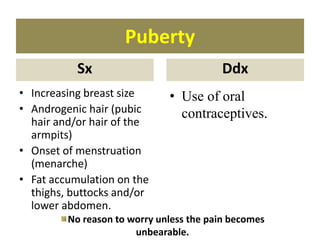
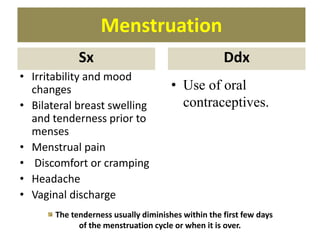
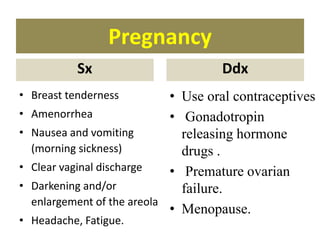
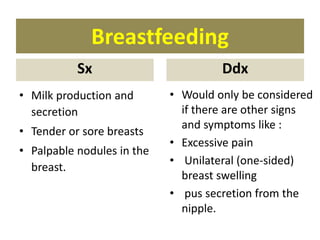
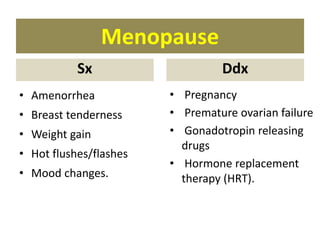
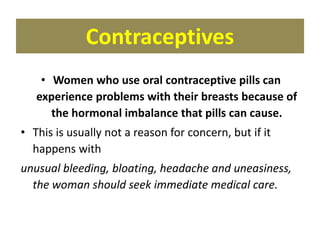
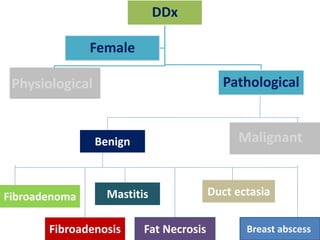
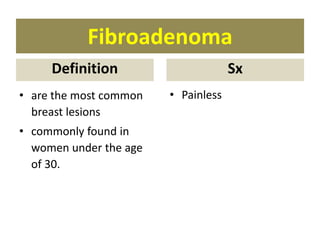
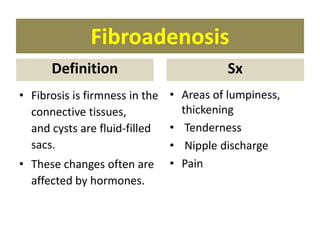
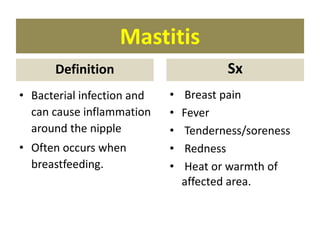
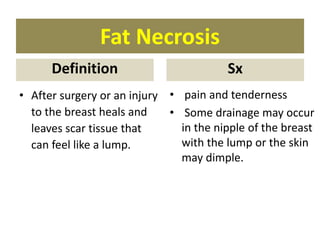
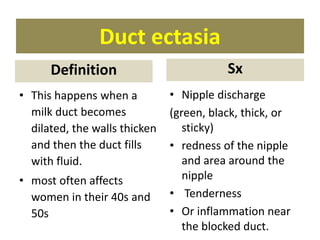
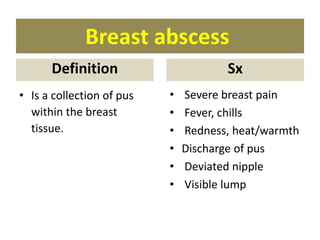
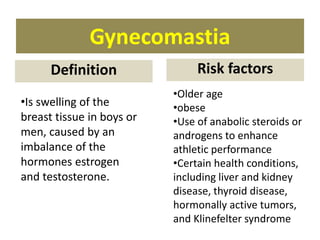
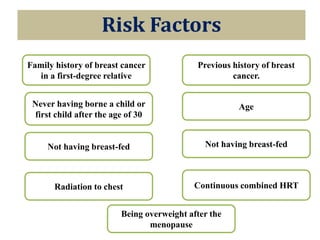
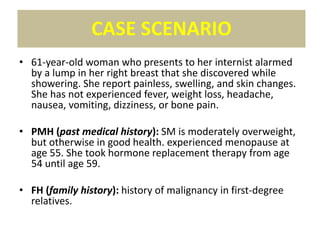
- Differential diagnoses of breast swelling including physiological causes like puberty, menstruation, pregnancy, breastfeeding, menopause, and contraceptives. Pathological causes include fibroadenoma, fibroadenosis, mastitis, fat necrosis and more.
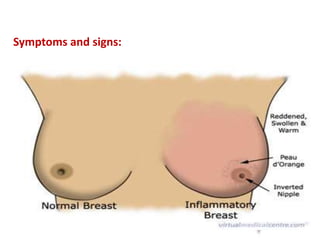
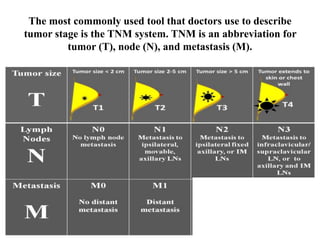
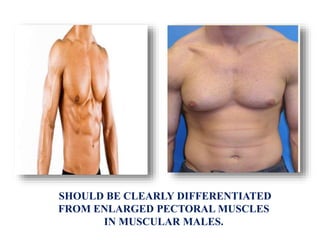
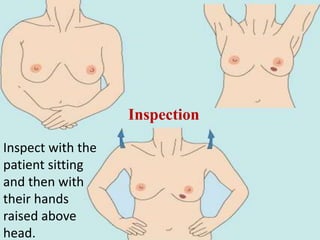
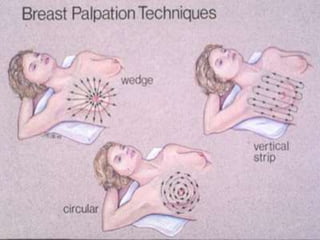
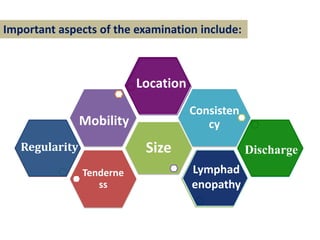
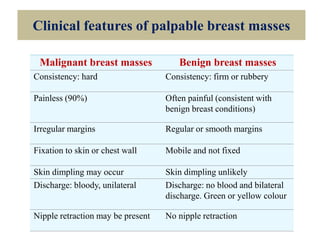
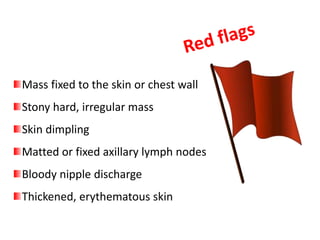
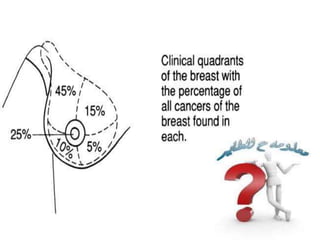
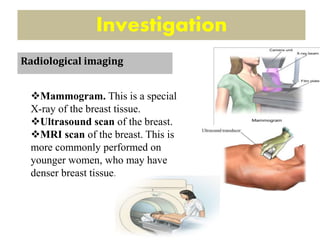
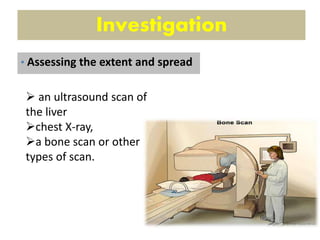
- Clinical evaluations for breast swelling including history, physical examinations, and investigations like mammograms, ultrasounds, biopsies and blood tests.
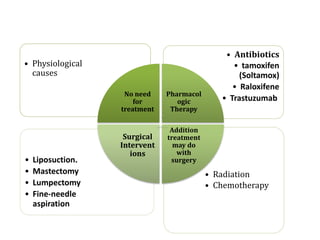
- Management of breast swelling depends on the underlying cause and may include observation, medications, surgery, radiation or chemotherapy.