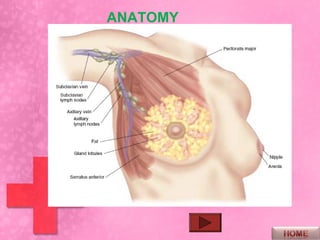
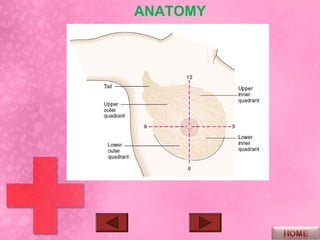
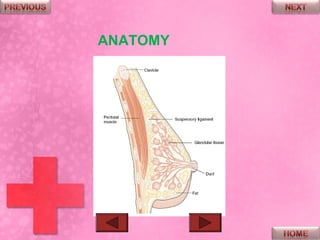
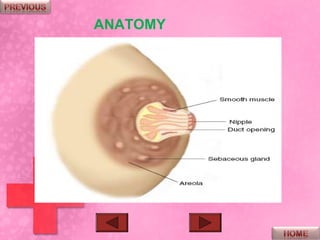
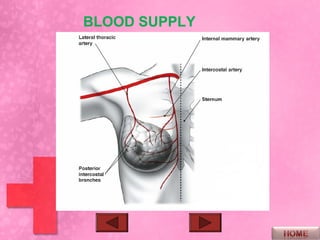
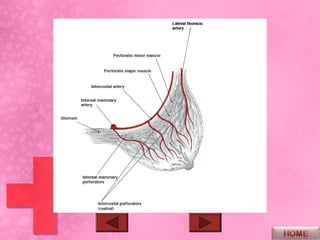
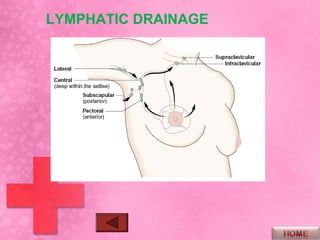
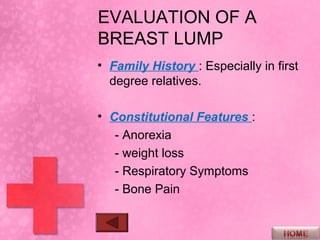
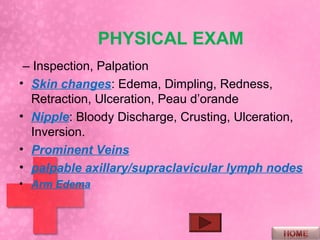
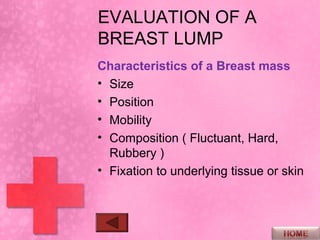
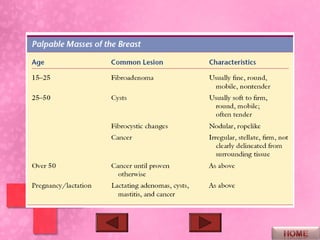
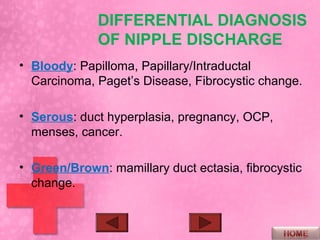
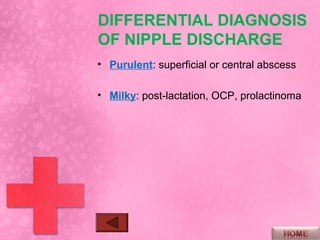
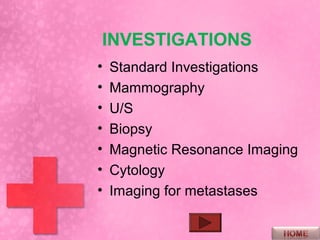
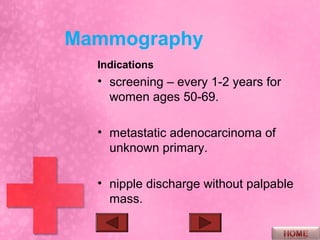
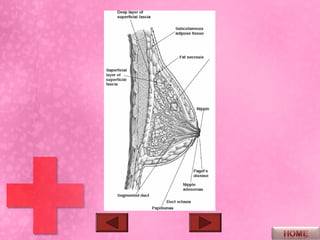
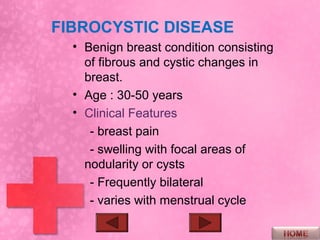
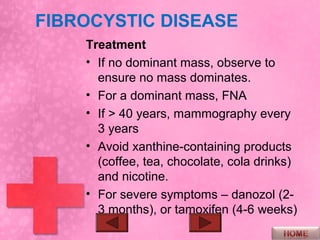
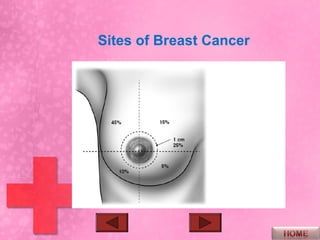
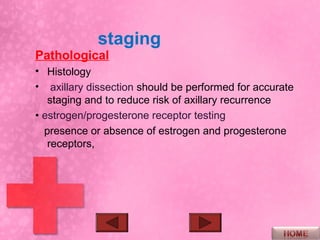
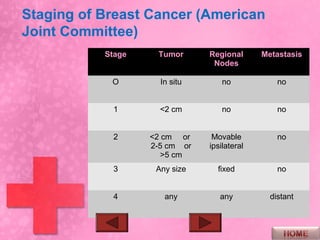
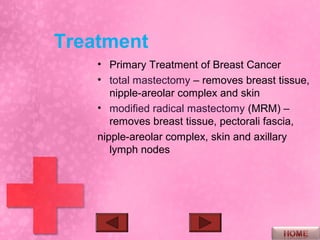
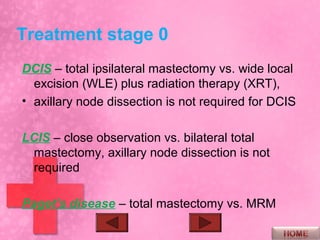
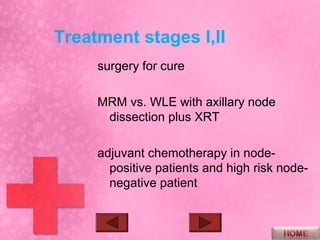
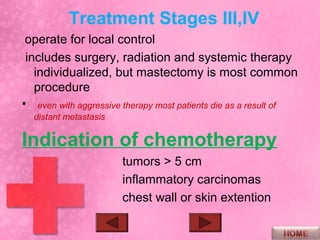
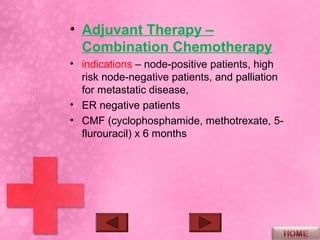
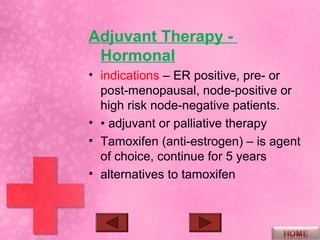
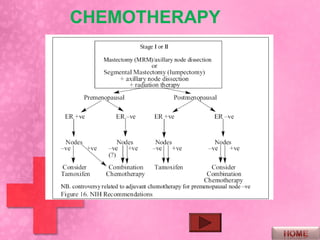
This document discusses the evaluation and differential diagnosis of breast lumps and nipple discharge. It begins by outlining the objectives, anatomy, history, and physical exam findings relevant to evaluating a patient with a breast lump or nipple discharge. It then reviews the differential diagnosis for breast lumps and types of nipple discharge. Investigations like mammography, ultrasound, and biopsy are discussed. Common benign breast conditions like fibrocystic disease and fibroadenomas are also summarized. The document concludes with an overview of breast cancer including epidemiology, risk factors, pathology, staging, treatment, and prognosis.