This document summarizes information about breast carcinoma, including:
- Pakistan has the highest rate of breast cancer in Asia, with approximately 90,000 new cases diagnosed annually.
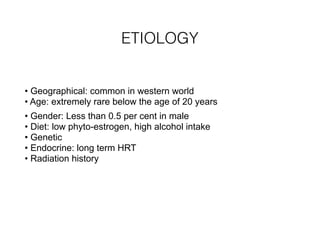
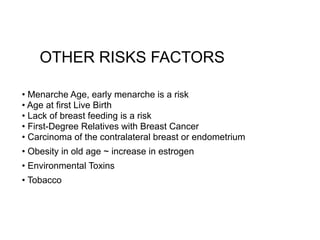
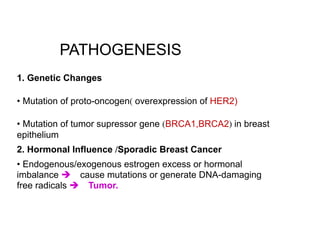
- Common risk factors include age, family history, obesity, lack of breastfeeding, and environmental toxins.
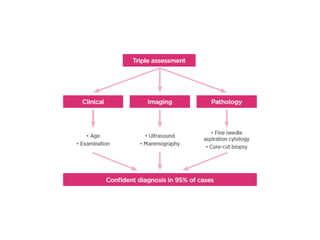
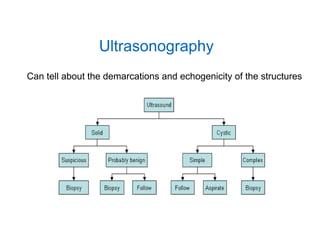
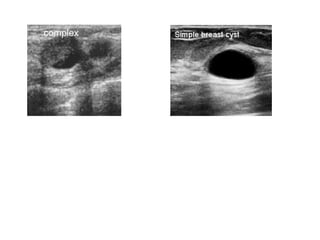
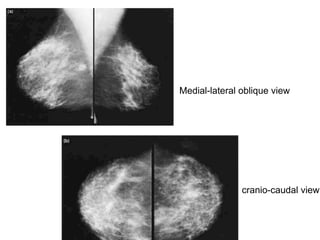
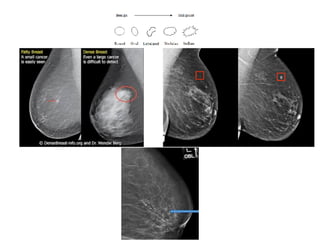
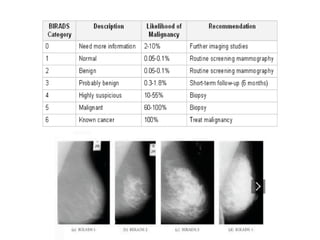
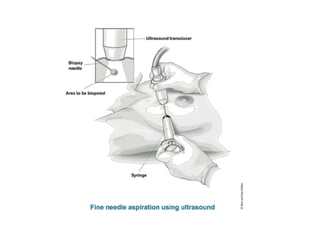
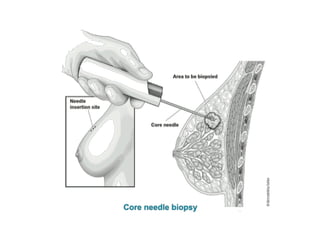
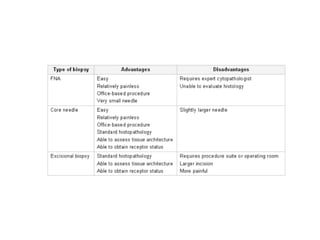
- Screening is recommended annually with mammography after age 40. Diagnosis involves biopsy of suspicious lumps.
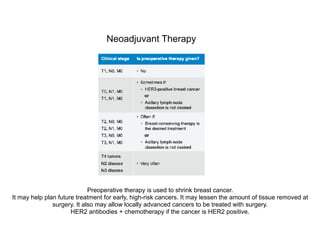
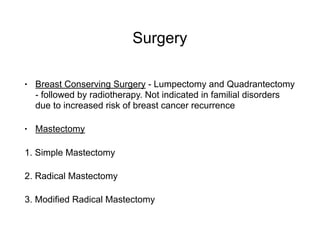
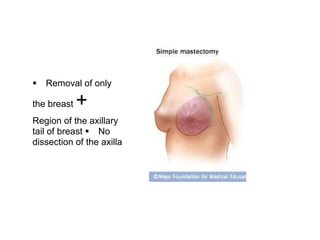
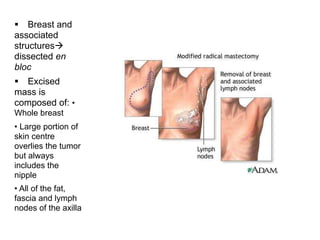
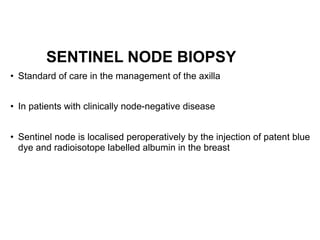
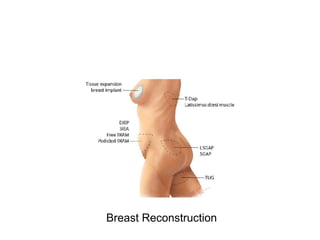
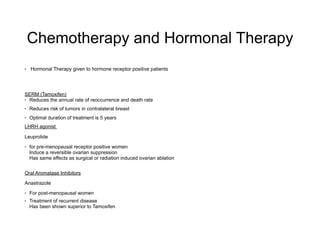
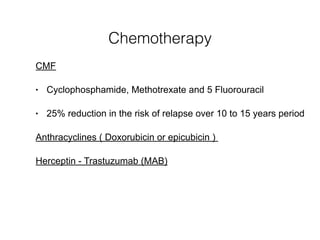
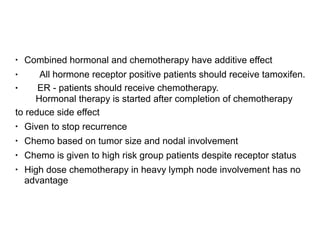
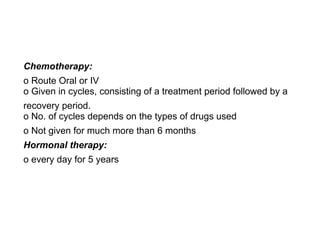
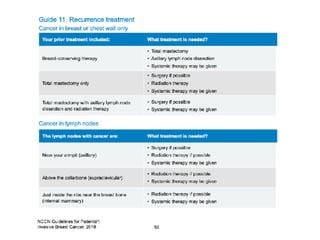
- Treatment options include surgery, chemotherapy, radiation therapy, hormone therapy, and reconstruction as needed.