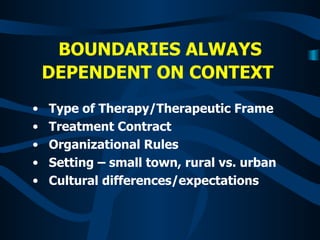
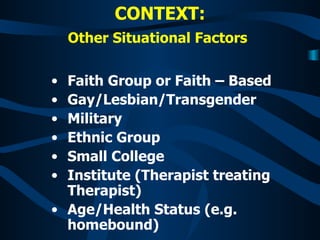
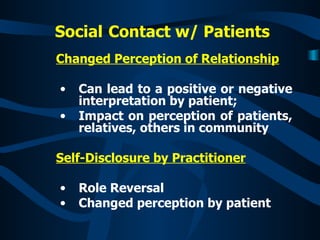
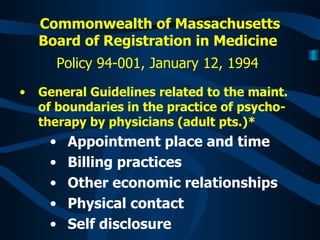
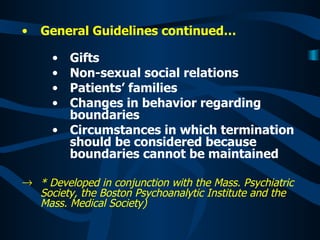
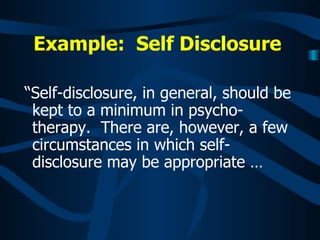
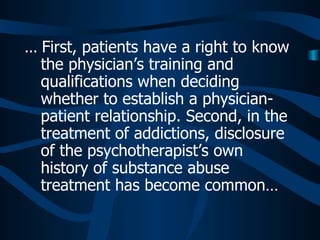
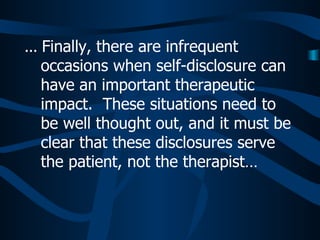
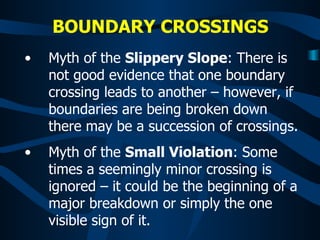
Professional boundaries in therapy are dependent on context and can vary based on factors like treatment setting, cultural differences, and situational factors of both the client and therapist. Boundary crossings occur when these boundaries become blurred and can be interpreted positively or negatively by clients. While some self-disclosure may be appropriate in certain circumstances like addiction treatment, therapists must ensure any disclosures are for the client's benefit and not their own. Maintaining clear boundaries is important to preserve the therapeutic relationship.
![WHAT ARE BOUNDARIES? “ Professional boundaries in medical practice are not well defined. In general, they are the parameters that describe the limits of a fiduciary relationship in which one person (a patient) [or client] entrusts his or her welfare to another (a physician) [or professional], to whom a fee is [usually] paid for the provision of a service.”* *(Taken from Gabbard & Nadelson, “Professional Boundaries in the Physician-Patient Relationship” JAMA, May 10, 1995-Vol. 273, No. 18).](https://image.slidesharecdn.com/boundariescrossing-120118175744-phpapp02/85/Boundaries-Crossing-2-320.jpg)