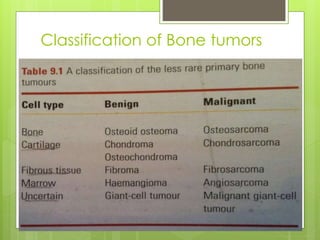
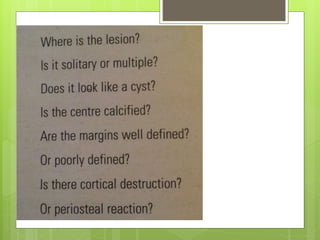
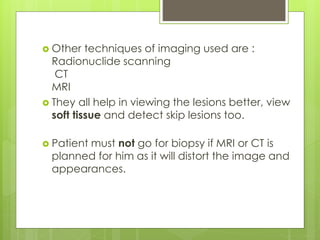
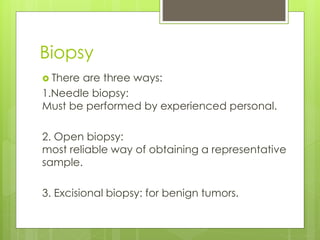
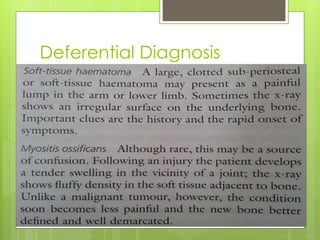
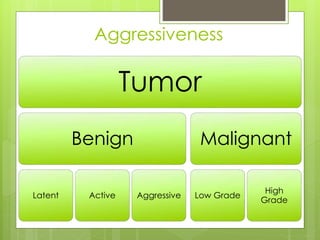
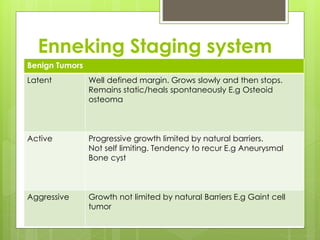
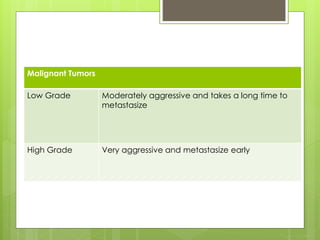
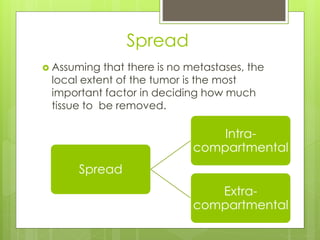
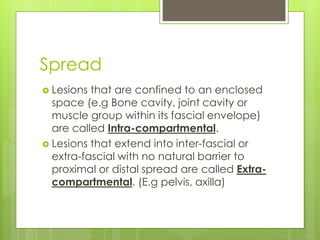
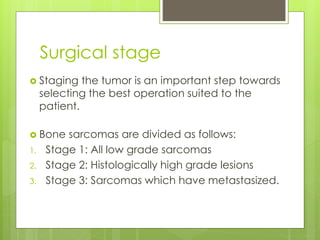
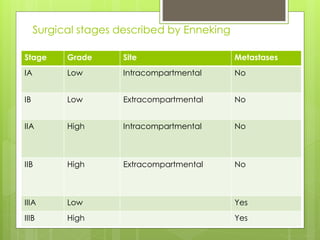
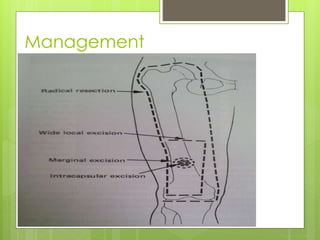
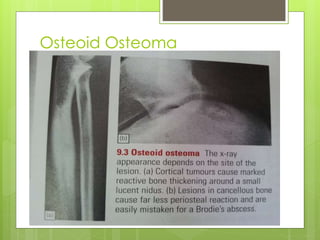
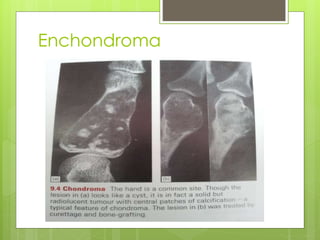
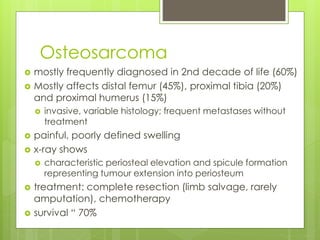
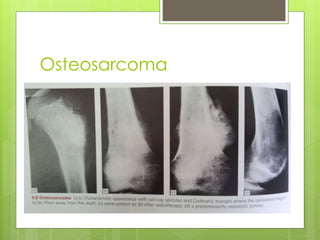
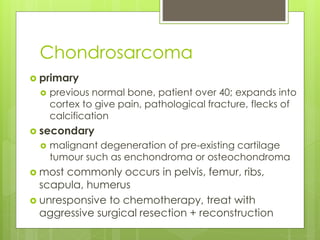
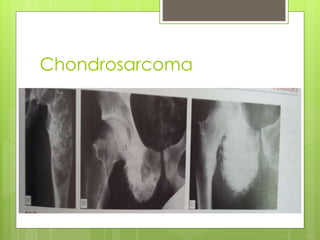
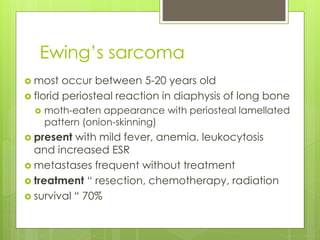
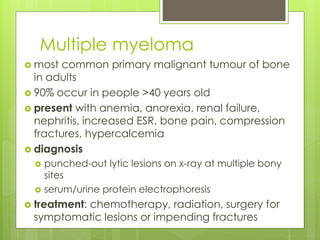
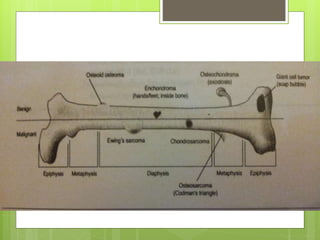
This document provides an overview of the approach to orthopedic oncology. It begins with an introduction and outlines the classification, clinical presentation, staging, and types of primary bone tumors. Bone tumors are classified based on the dominant tissue and can be benign or malignant. Clinical evaluation involves history, physical exam, imaging, and biopsy. Staging uses the Enneking system to describe the grade, site, and presence of metastases. Primary bone tumors discussed include benign entities like osteoid osteoma and giant cell tumor as well as malignant tumors such as osteosarcoma, Ewing's sarcoma, and chondrosarcoma. Treatment depends on the tumor type, location, and stage.