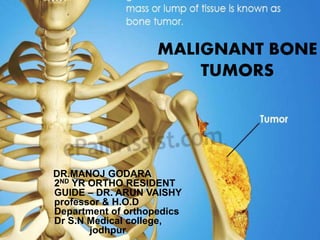
1. Malignant bone tumors are aggressive cancers that rapidly destroy tissue and commonly spread to other areas. They make up about 0.5% of all cancers.
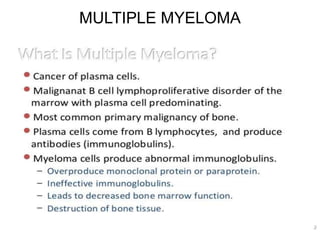
2. The most common malignant bone tumors are metastases from other primary cancers, which account for 70% of cases. Primary bone cancers include osteosarcoma, chondrosarcoma, and Ewing's sarcoma.
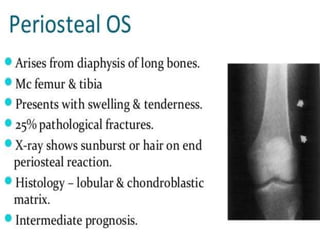
3. Diagnosis involves imaging like x-rays, CT, and MRI to identify bone destruction and tumor extent. Biopsy is needed for histological examination to determine the tumor type and grade. Treatment depends on the cancer but commonly involves surgery along with chemotherapy and radiation.