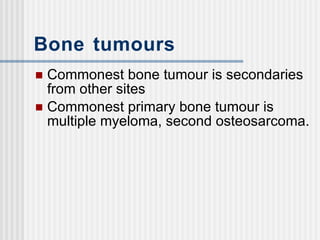
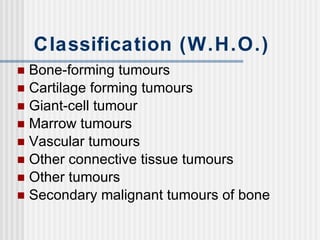
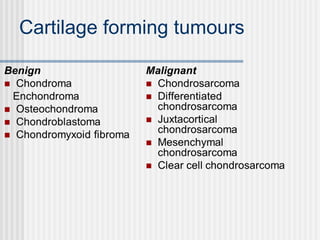
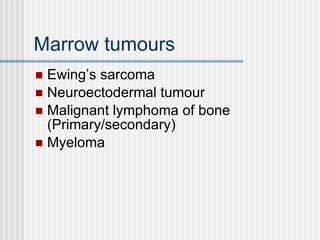
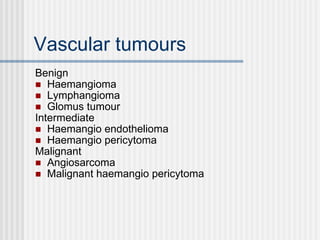
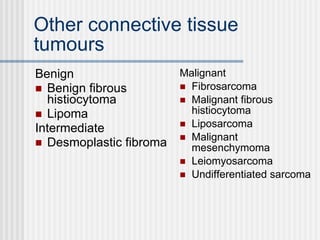
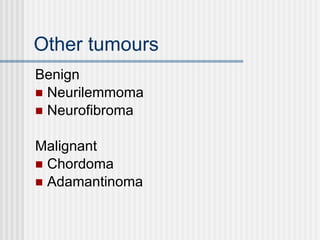
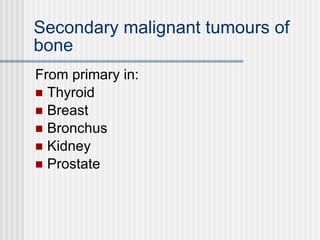
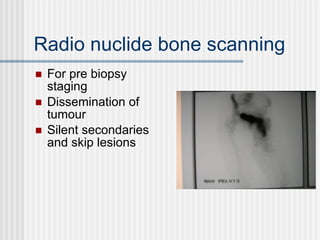
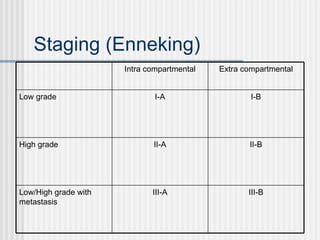
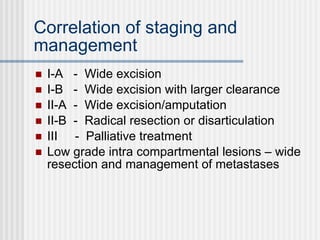
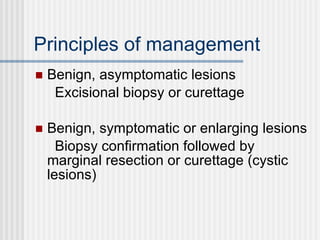
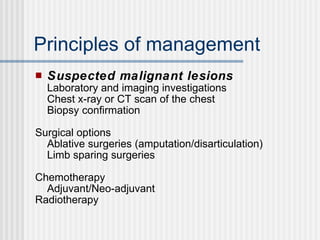
The document discusses bone tumors. It begins by stating that the most common bone tumor is secondary tumors from other sites, while the most common primary bone tumor is multiple myeloma. It then covers the WHO classification of bone tumors including bone-forming, cartilage-forming, marrow, vascular, and other tumors. Diagnosis involves clinical examination, imaging like radiographs, CT, MRI and bone scans, as well as laboratory tests and biopsy. Staging is discussed including the Enneking system based on aggressiveness and spread. Management depends on staging and includes wide excision for low grade lesions and more radical resection or palliative treatment for high grade or metastatic tumors.