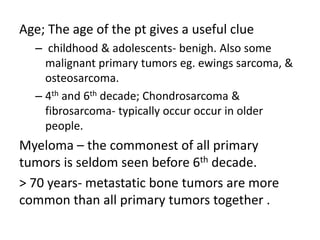
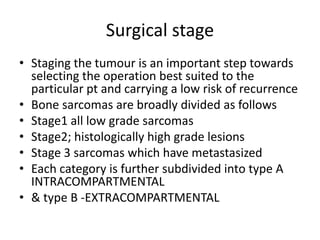
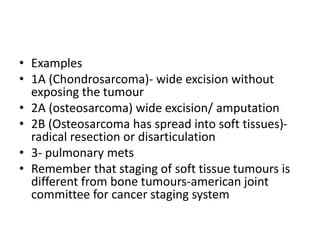
This document discusses bone tumors, including classification, clinical features, diagnosis, and treatment. It covers both benign and malignant tumors. Benign tumors are more common and often asymptomatic, while primary malignant tumors are rare but can be aggressive. Diagnosis involves medical history, physical exam, radiological imaging like X-ray and MRI, and biopsy. Treatment depends on tumor type, grade, and stage, and may include surgical excision, chemotherapy, or limb salvage versus amputation for malignant tumors. The goal is wide excision for local control while minimizing damage and recurrence risks.