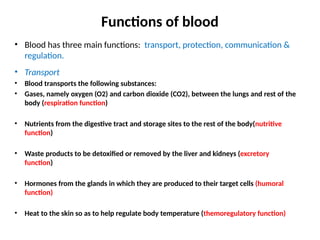
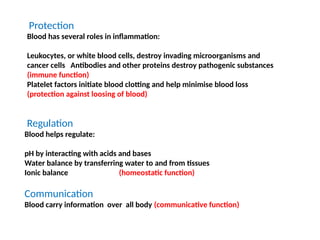
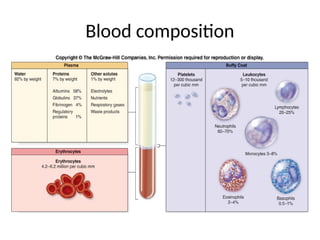
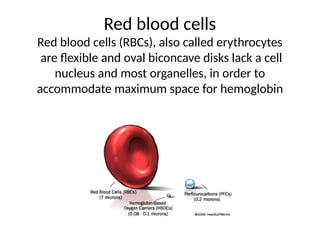
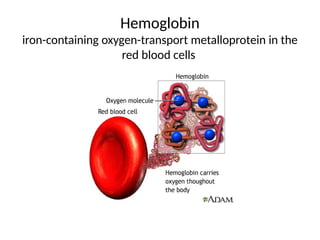
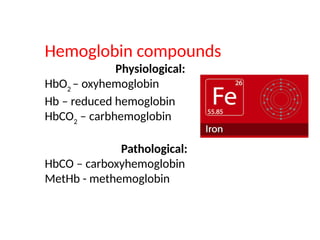
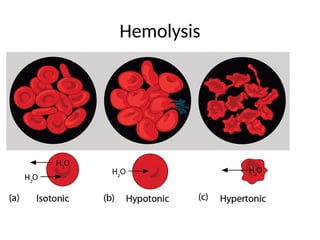
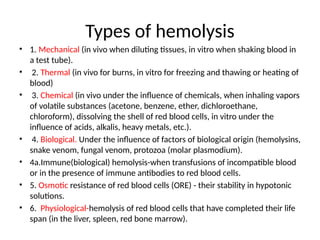
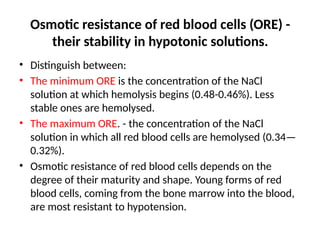
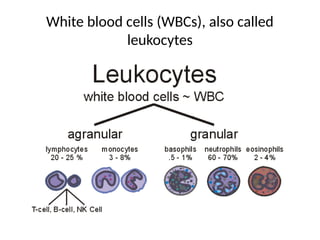
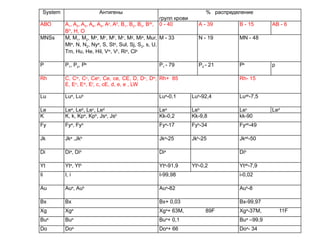
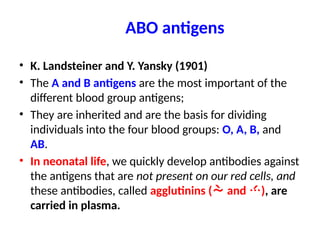
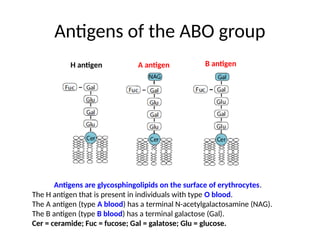
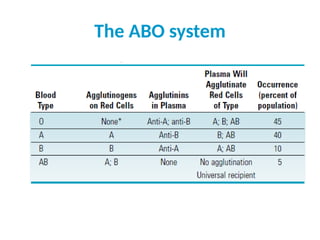
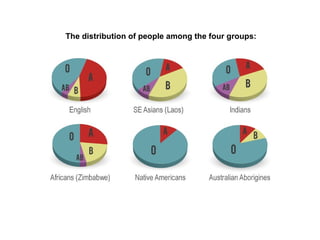
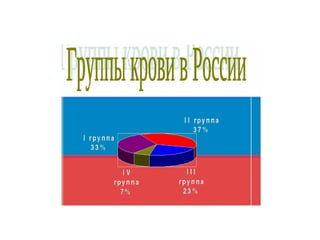
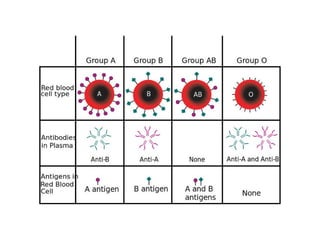
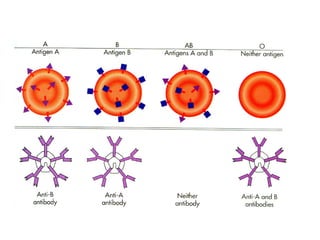
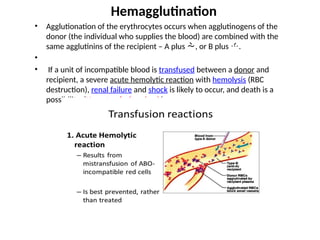
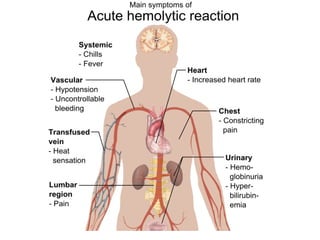
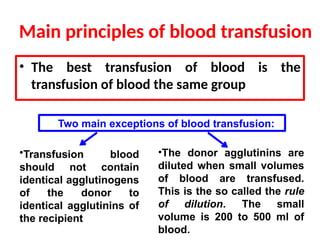
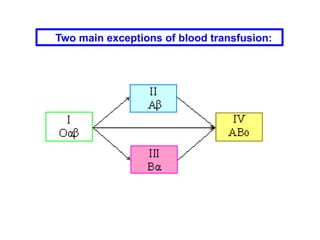
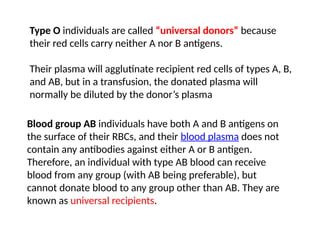
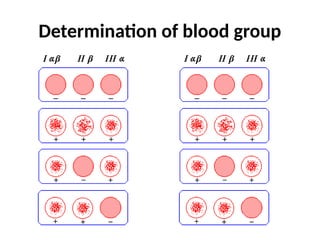
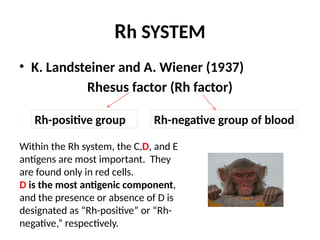
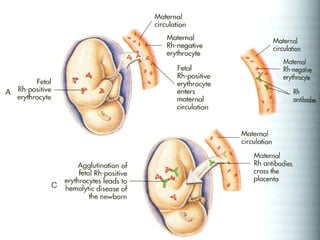
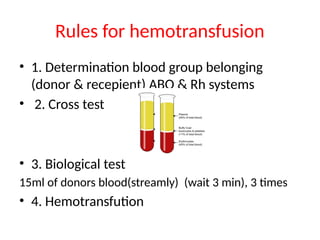
The document discusses the physiology and functions of blood, highlighting transport, protection, and regulation roles. It details blood composition, types of hemolysis, blood group systems, and the significance of ABO and Rh blood types in transfusions. It emphasizes the importance of matching donor and recipient blood types to prevent severe transfusion reactions.