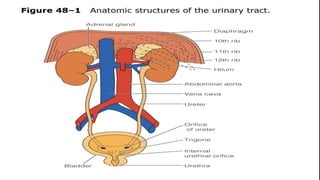
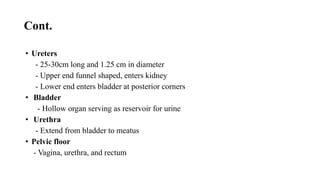
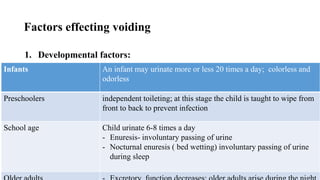
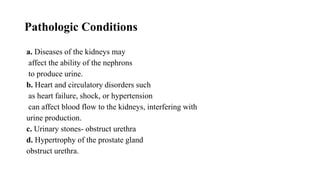
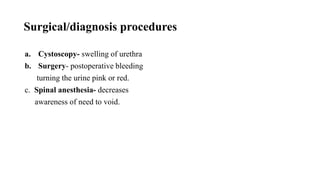
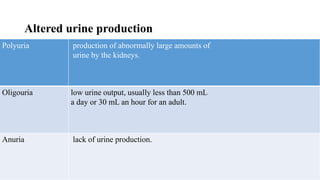
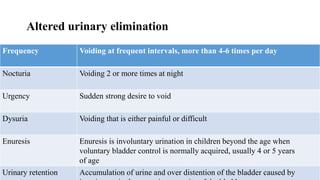
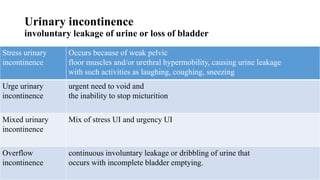
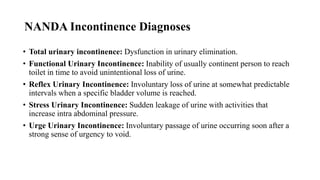
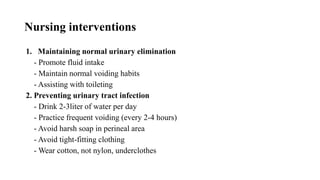
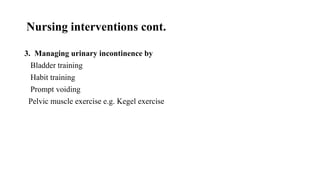
This document describes the physiology and process of urinary elimination, including urine formation in the kidneys and storage in the bladder. It identifies factors that can influence urination such as development, psychology, fluid intake, and medications. Common urinary problems like incontinence, retention, infection, and their nursing interventions are discussed. The goals of nursing care are maintaining normal elimination patterns, preventing infections, and managing incontinence through techniques like bladder training and Kegel exercises.