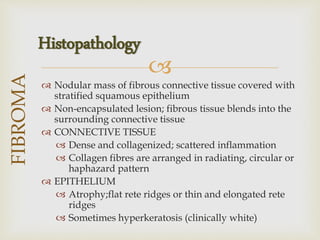
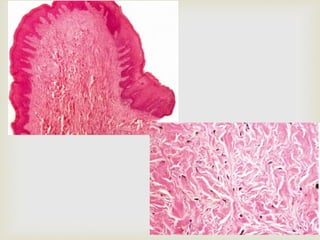
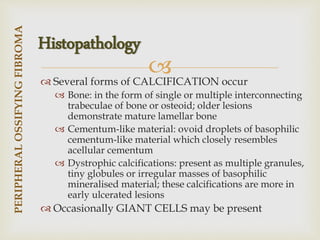
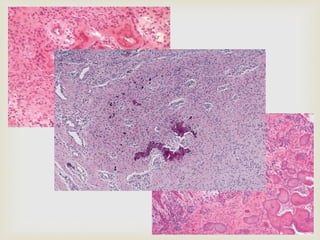
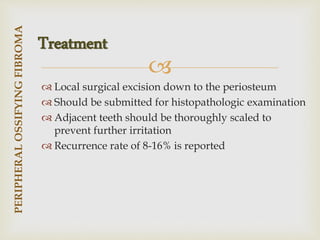
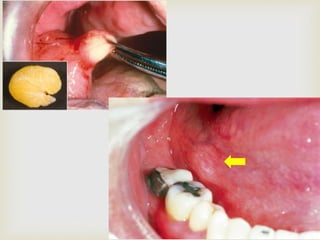
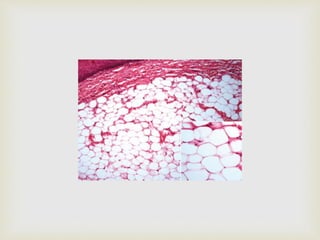
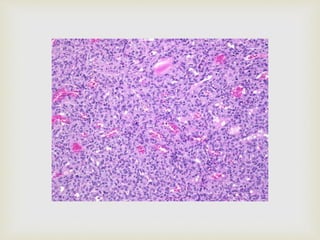
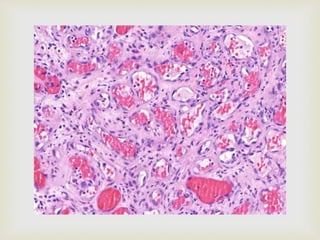
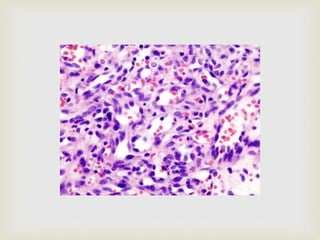
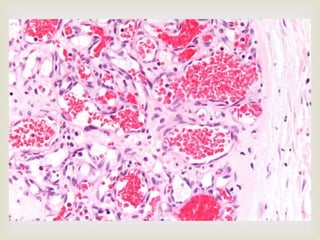
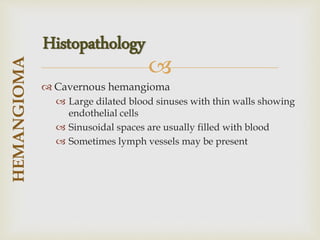
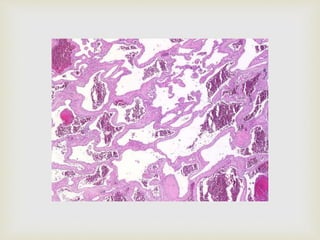
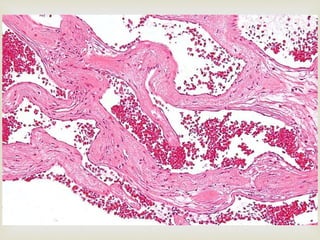
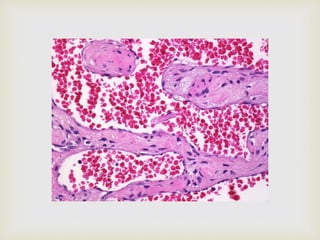
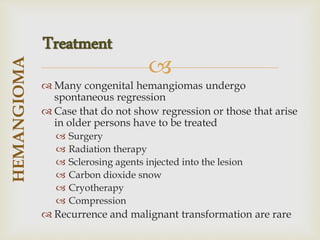
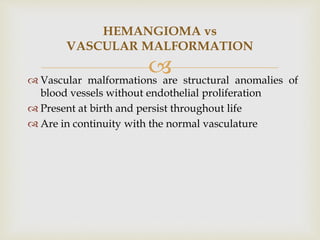
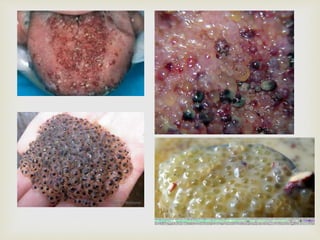
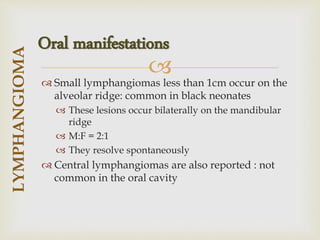
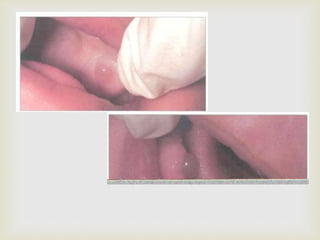
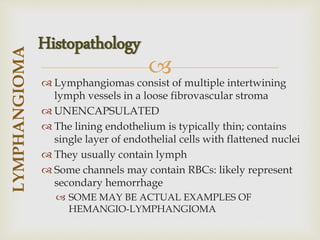
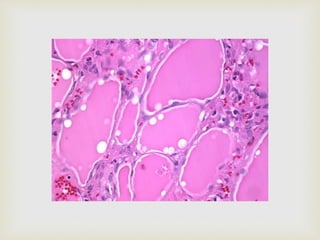
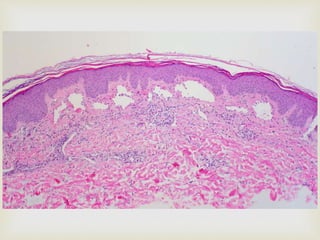
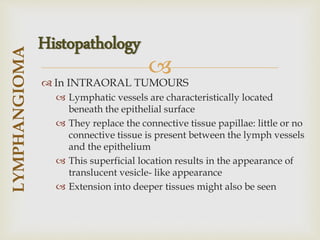
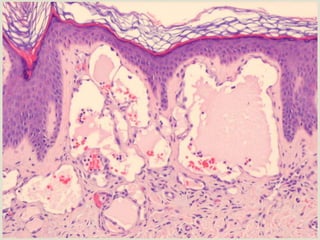
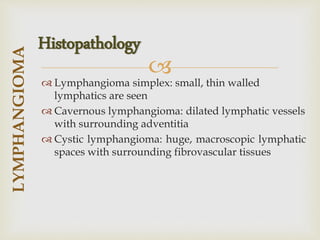
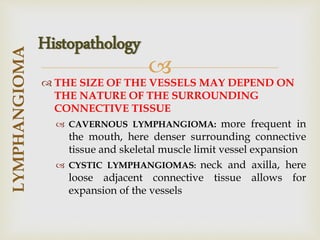
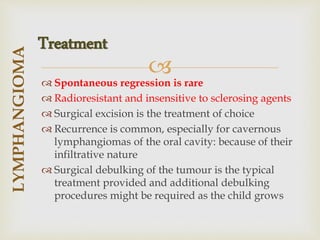
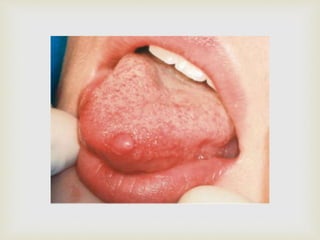
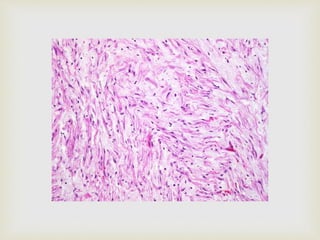
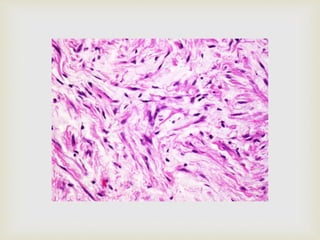
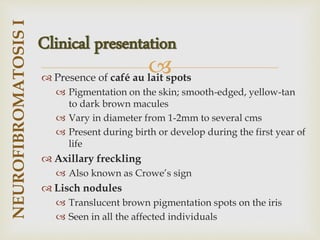
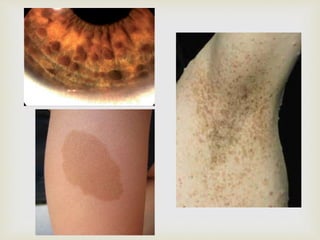
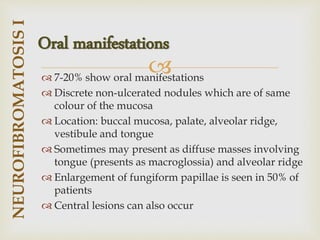
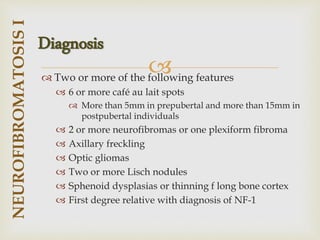
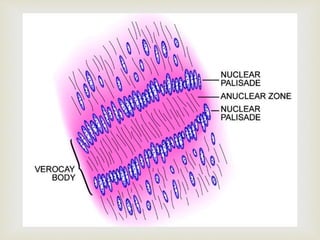
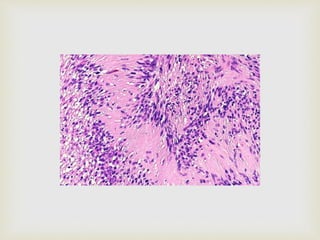
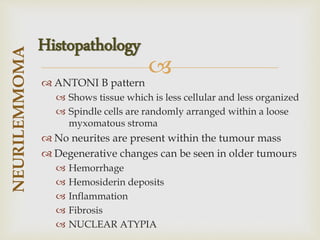
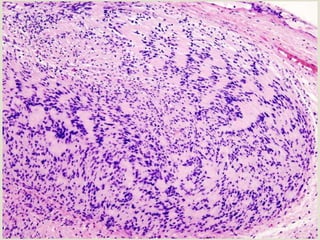
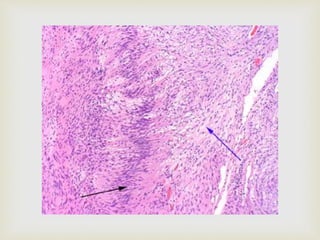
The document discusses various benign tumours, malignant tumours, and tumour-like lesions found in the oral cavity. It provides details on different types of benign tumours including fibroma, peripheral ossifying fibroma, lipoma, hemangioma, lymphangioma, neurilemmoma and neurofibroma. For each tumour, it describes clinical features, presentation, histopathology and treatment. It also discusses some common malignant tumours and tumour-like lesions such as central giant cell granuloma and aneurysmal bone cyst.