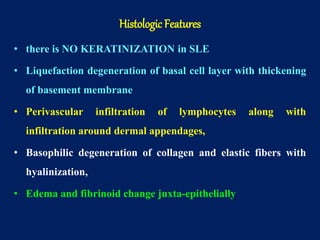
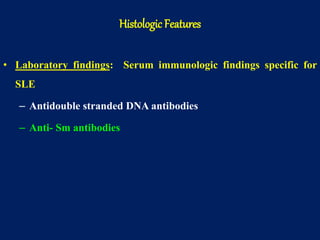
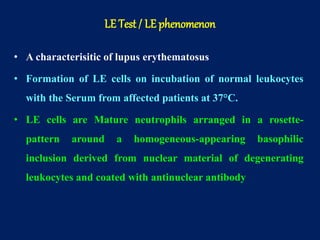
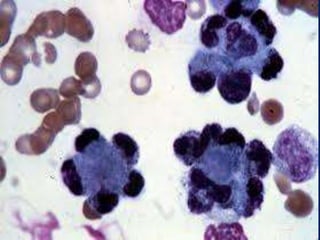
This document summarizes key information about systemic lupus erythematosus (SLE). It describes SLE as an autoimmune disease characterized by the formation of autoantibodies and immune complexes that can damage multiple organs like the kidneys, skin, blood cells, and central nervous system. Genetics, hormonal imbalances, and environmental factors can lead to immune dysregulation and the production of autoantibodies against nuclear and other antigens. SLE predominantly affects women aged 30-40 and can present with characteristic rashes and oral ulcers. Complications involve organ damage like glomerulonephritis. Diagnosis involves identifying clinical features and serum autoantibodies.