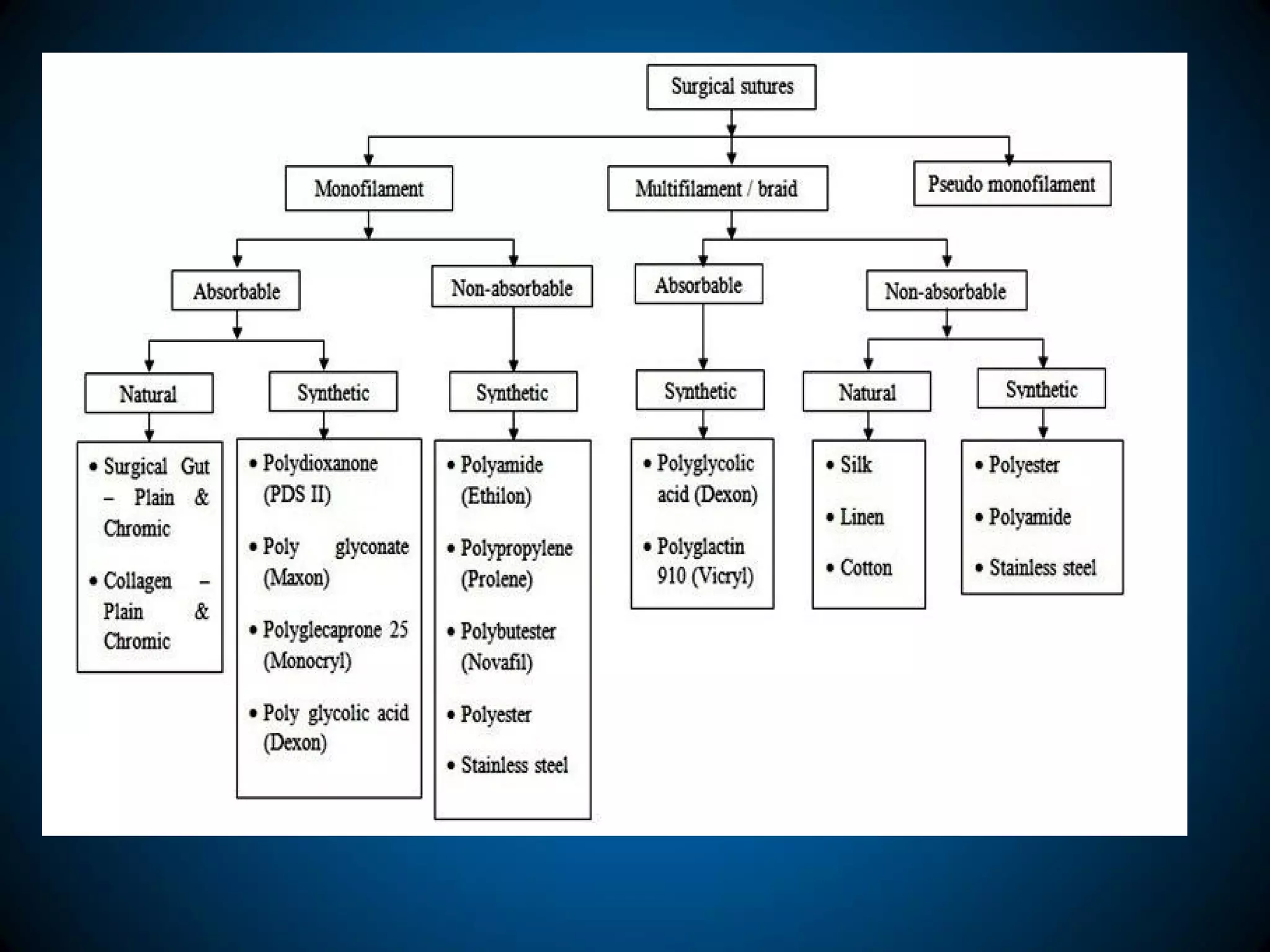
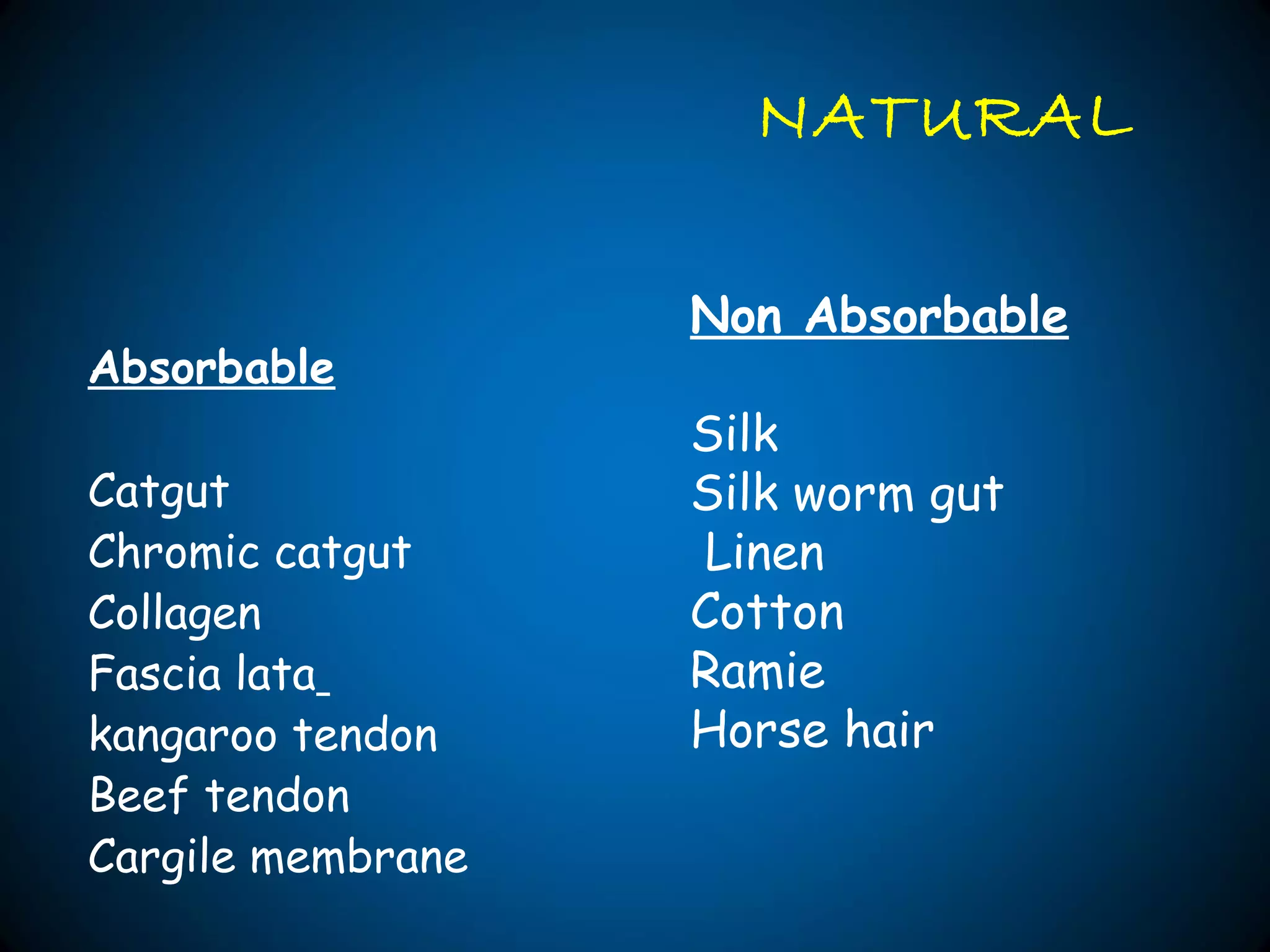
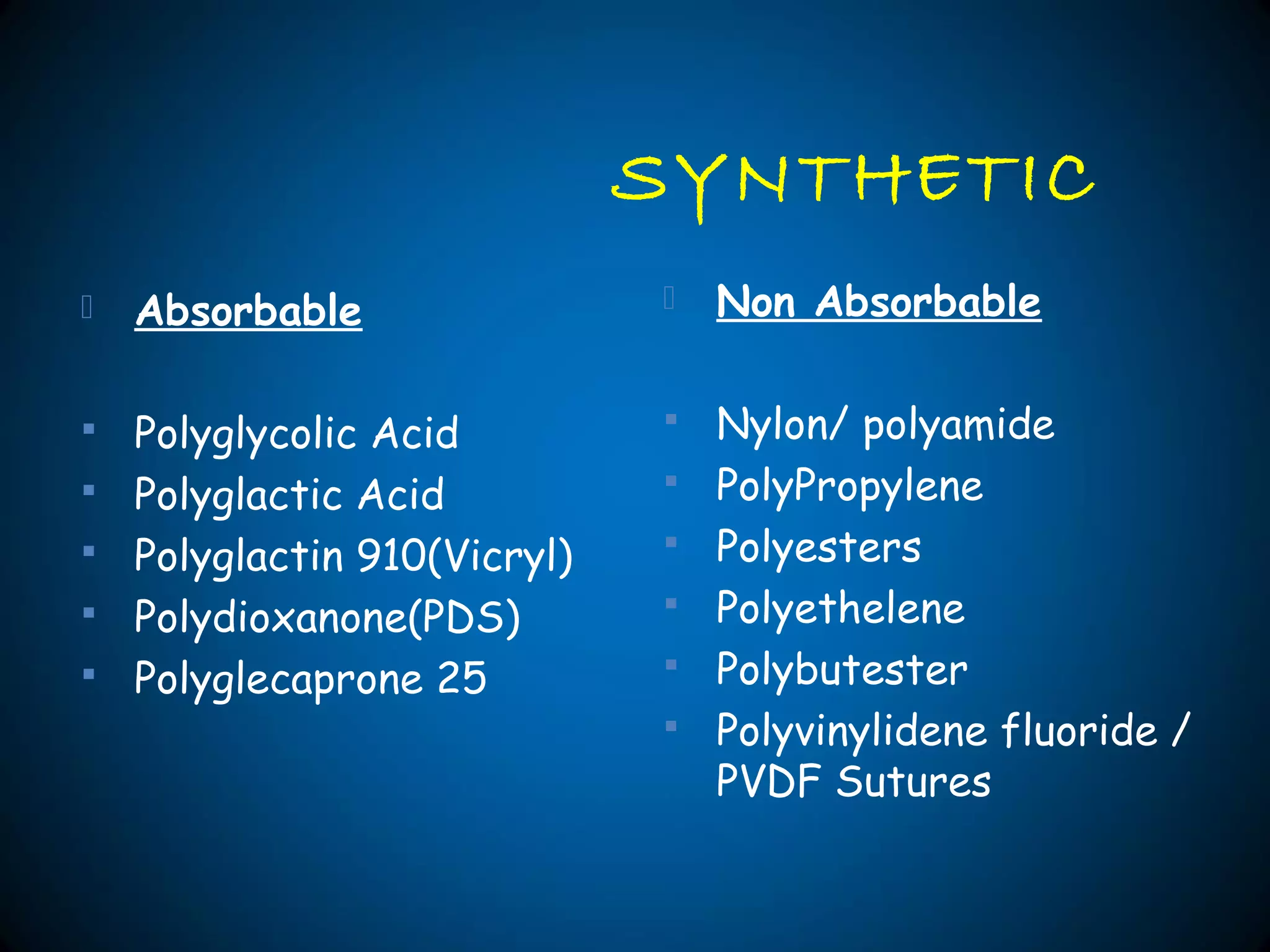
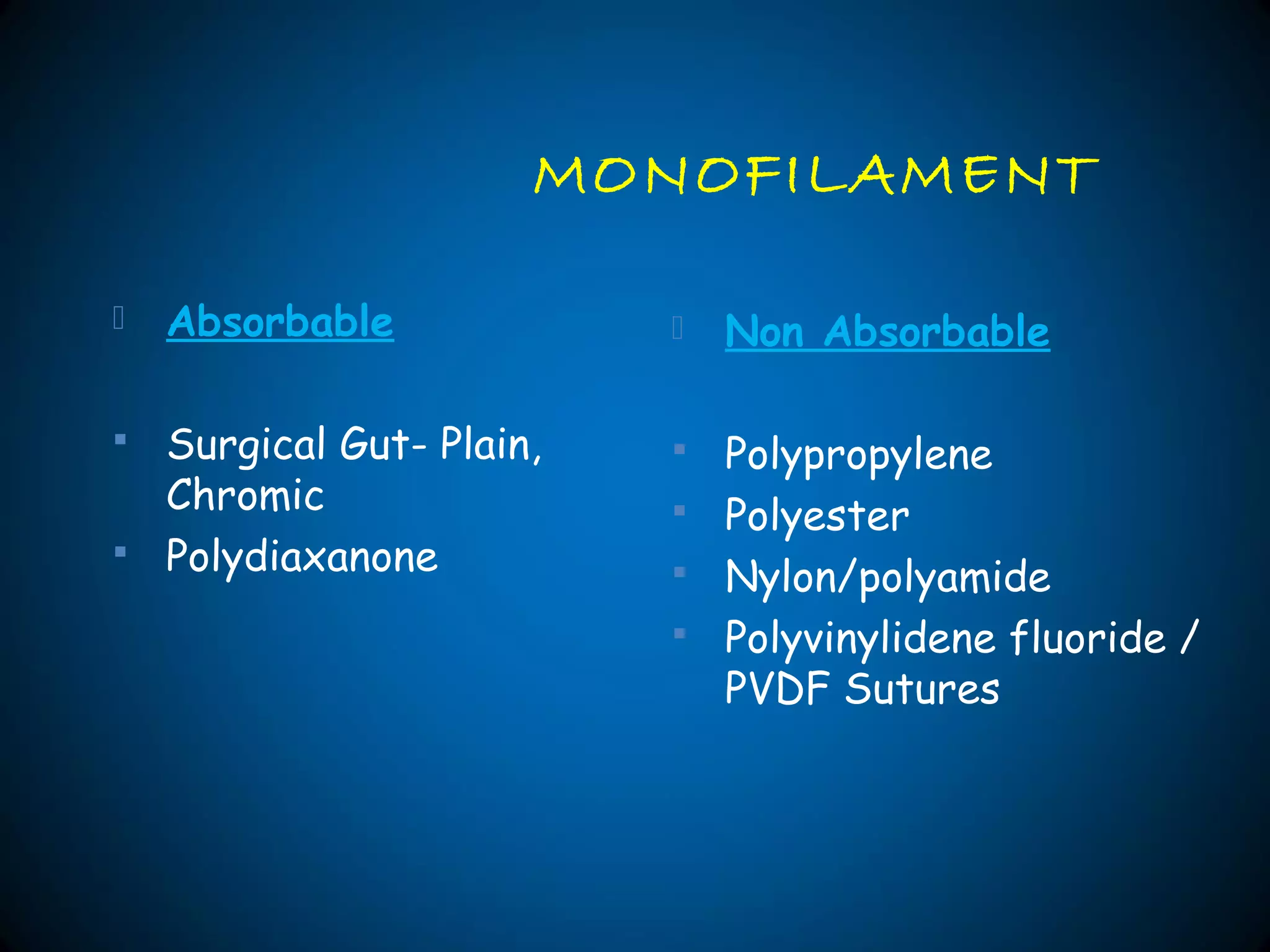
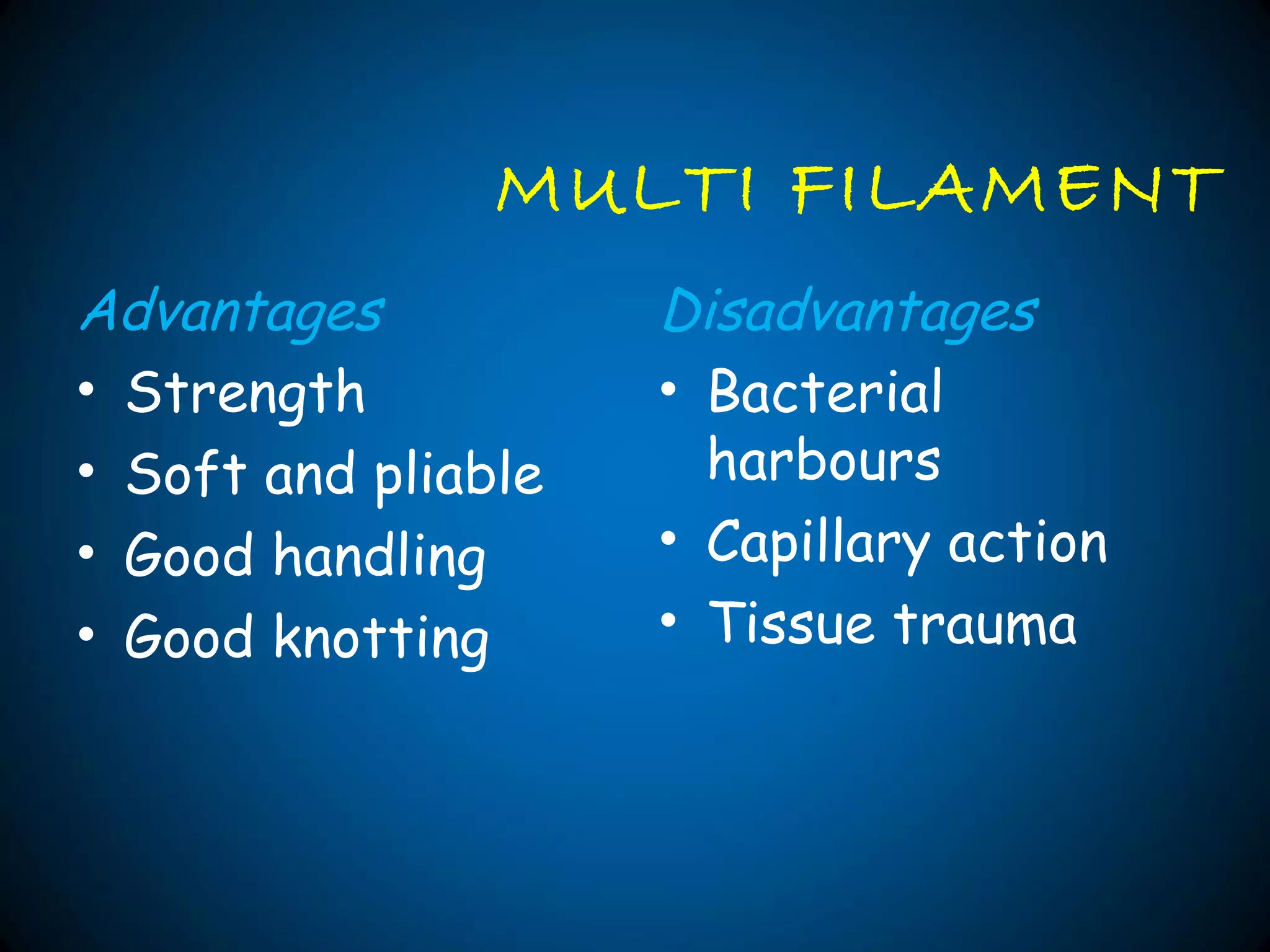
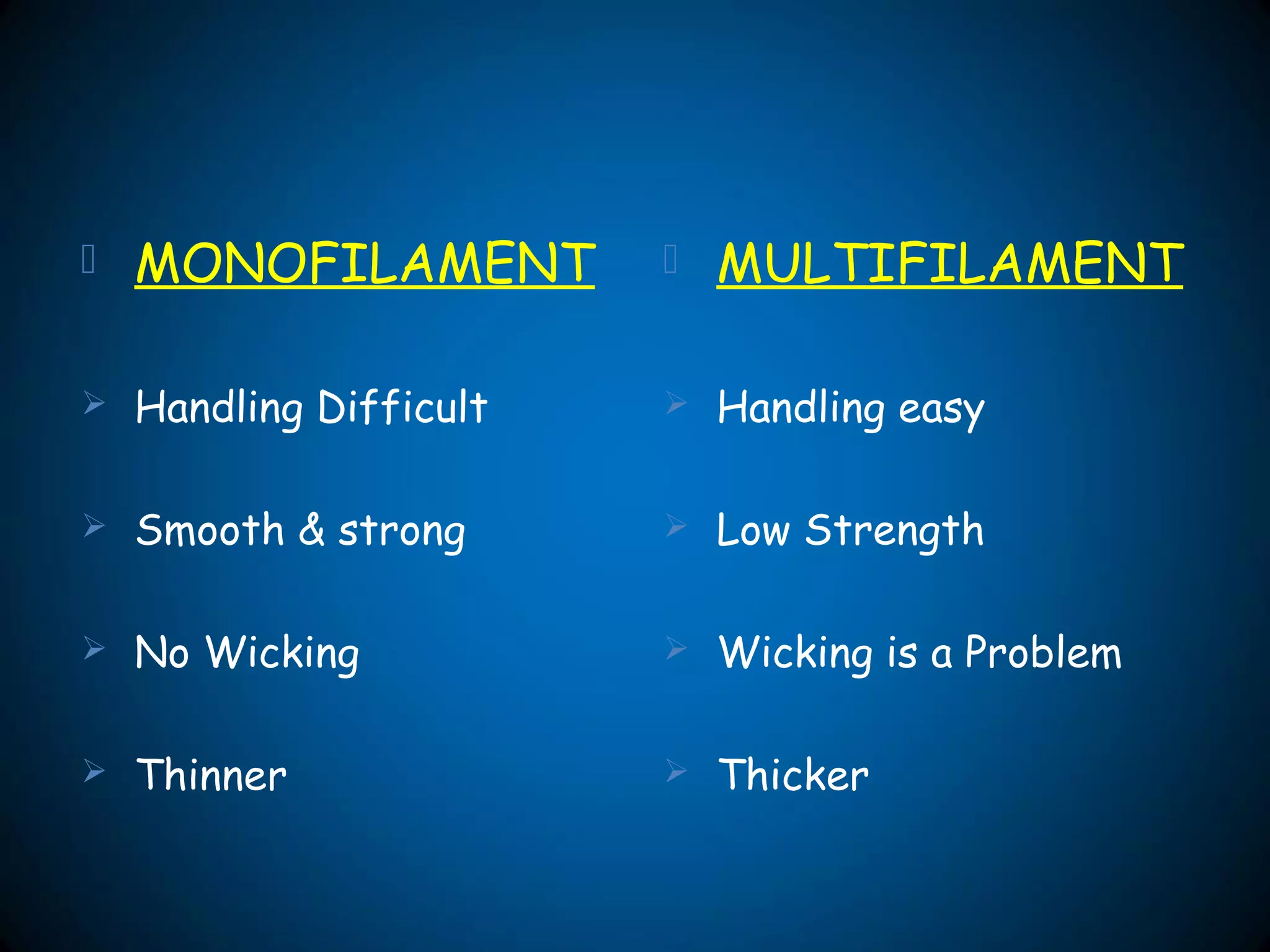
1. The document discusses different types of sutures including natural, synthetic, and metallic sutures. It describes properties of sutures such as absorption rate, tensile strength, and examples of common absorbable and non-absorbable suture materials.
2. Specific suture materials discussed in detail include gut, chromic catgut, polyglactin 910, polyglecaprone 25, polydioxanone, and surgical silk. Absorbtion rates, tensile strength, and indications for different materials are provided.
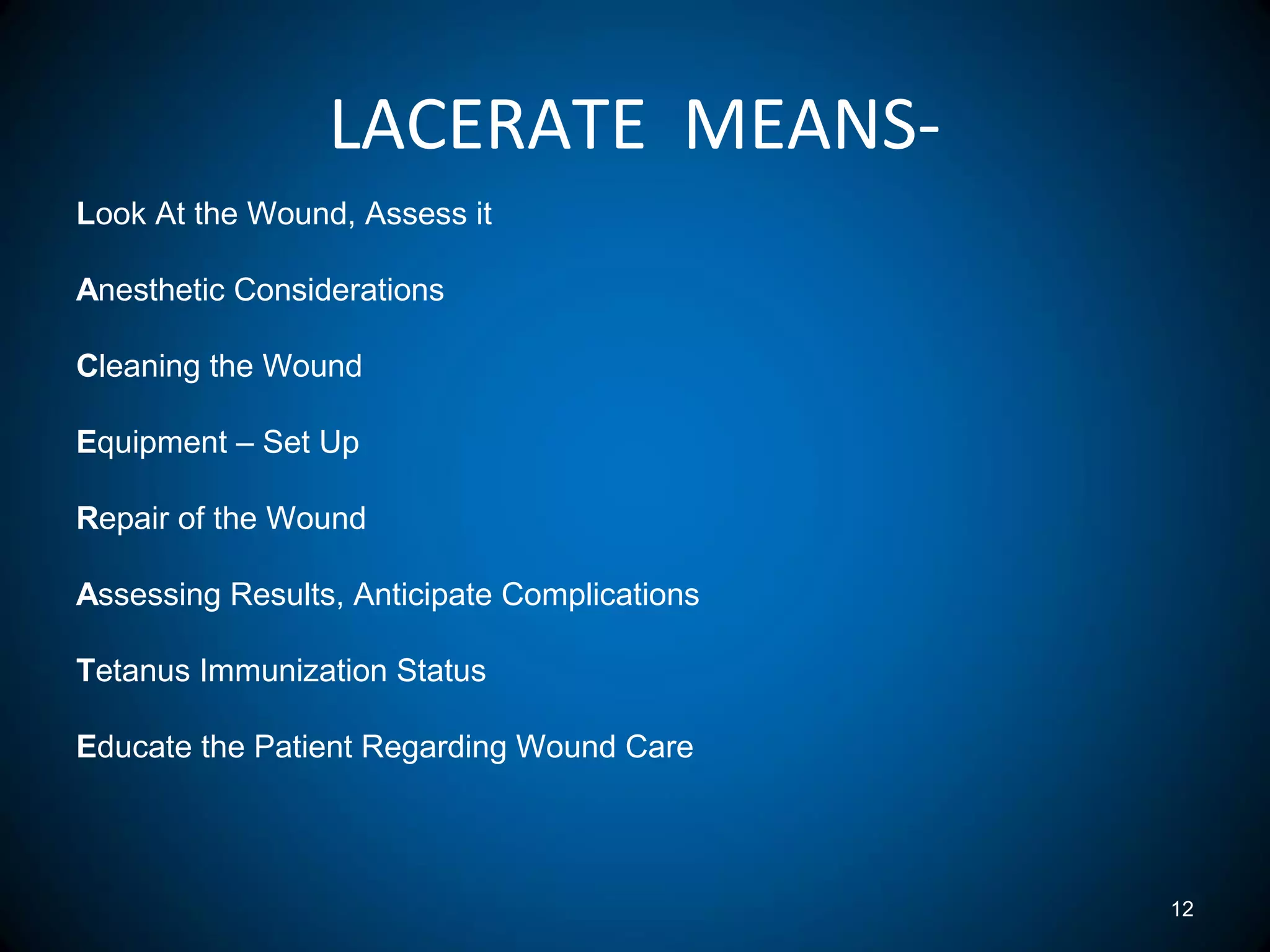
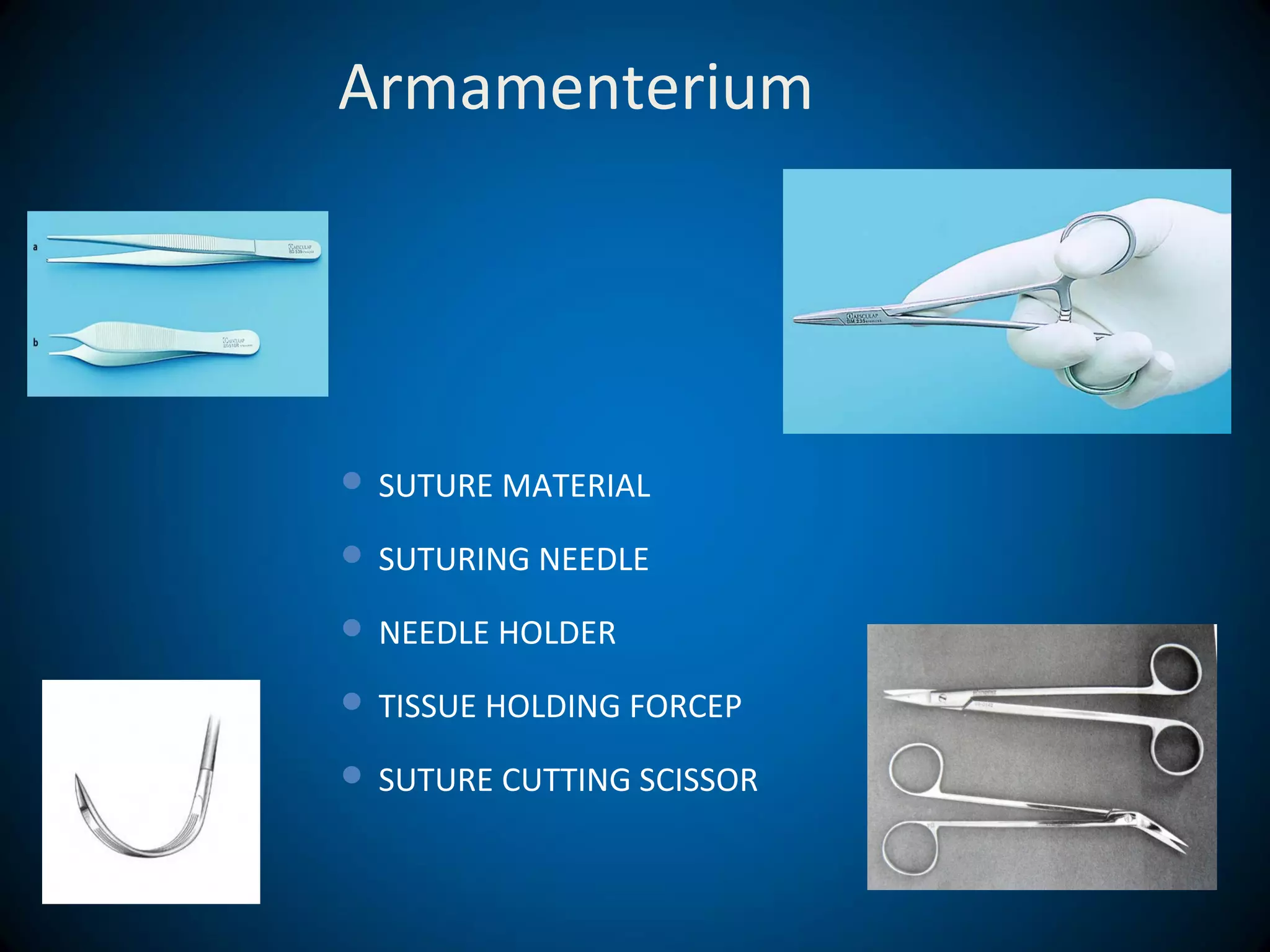
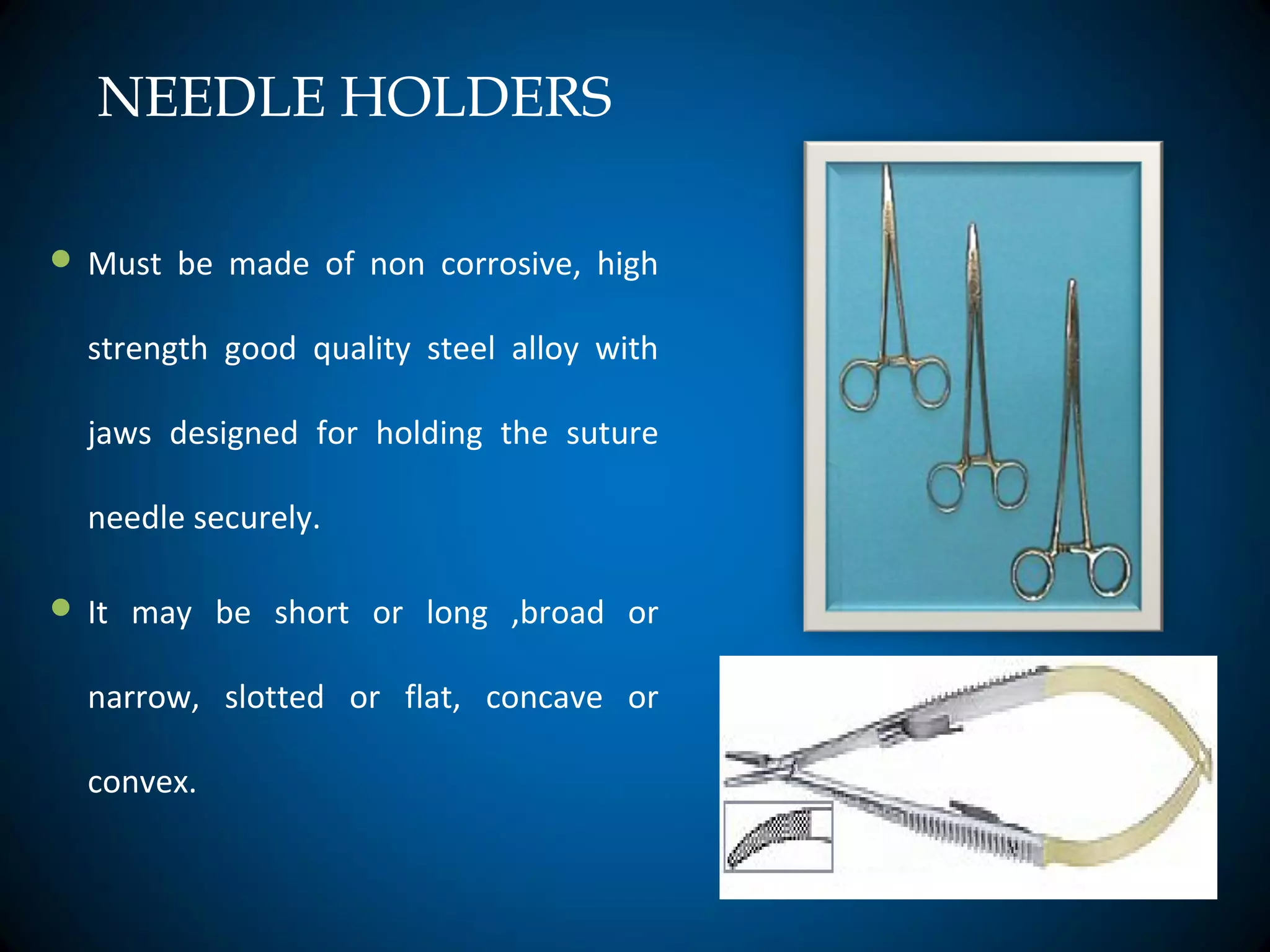
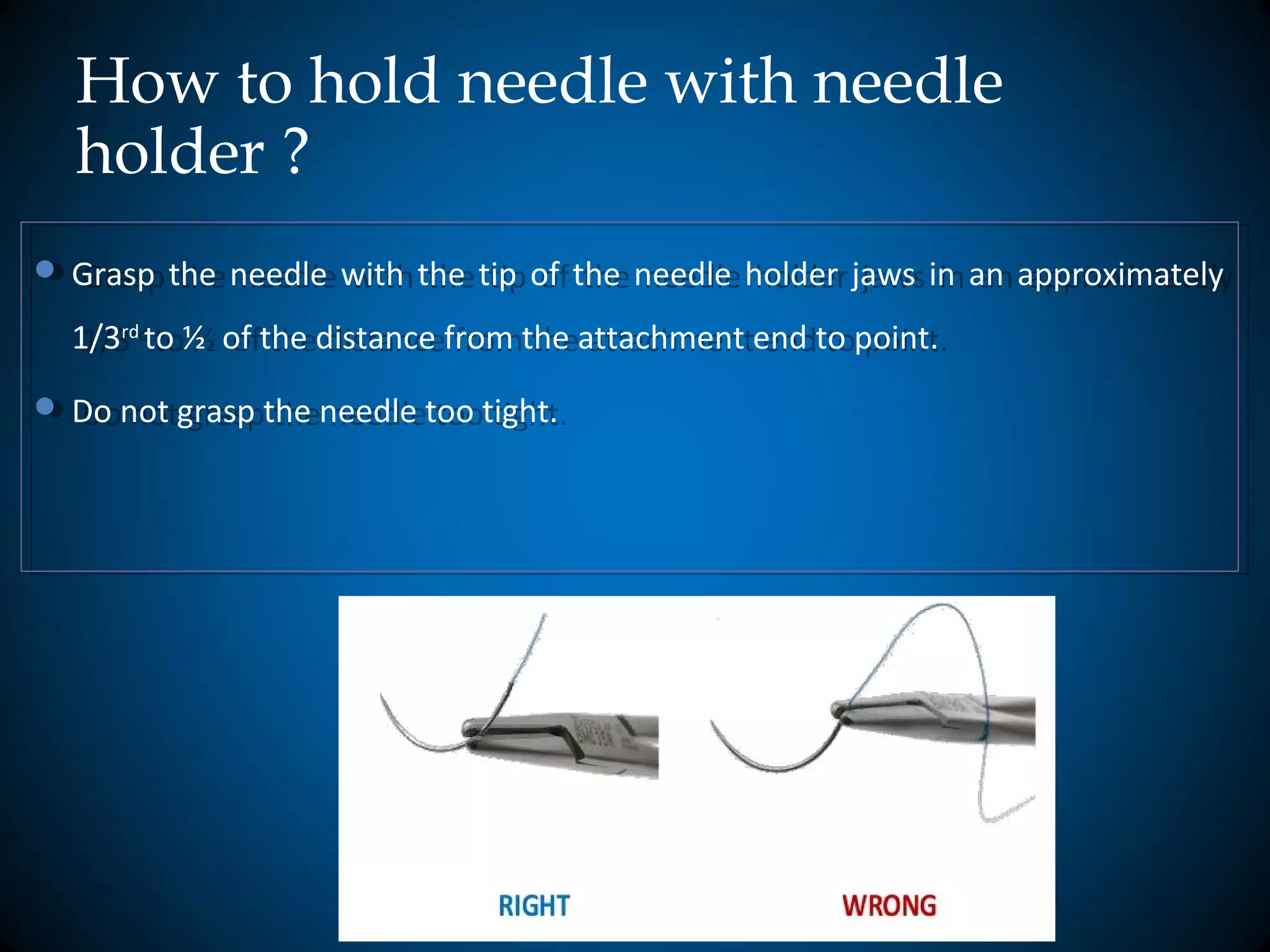
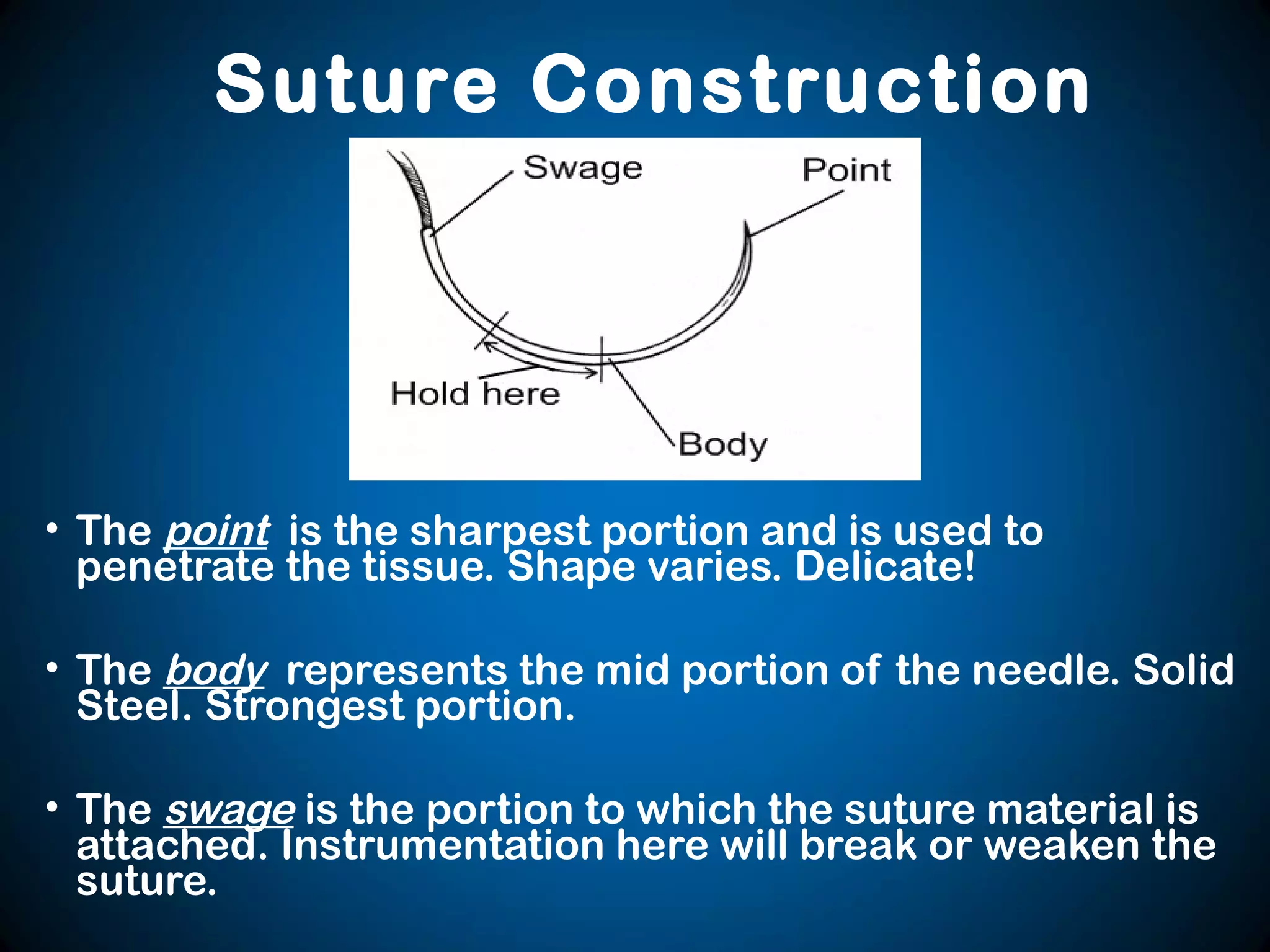
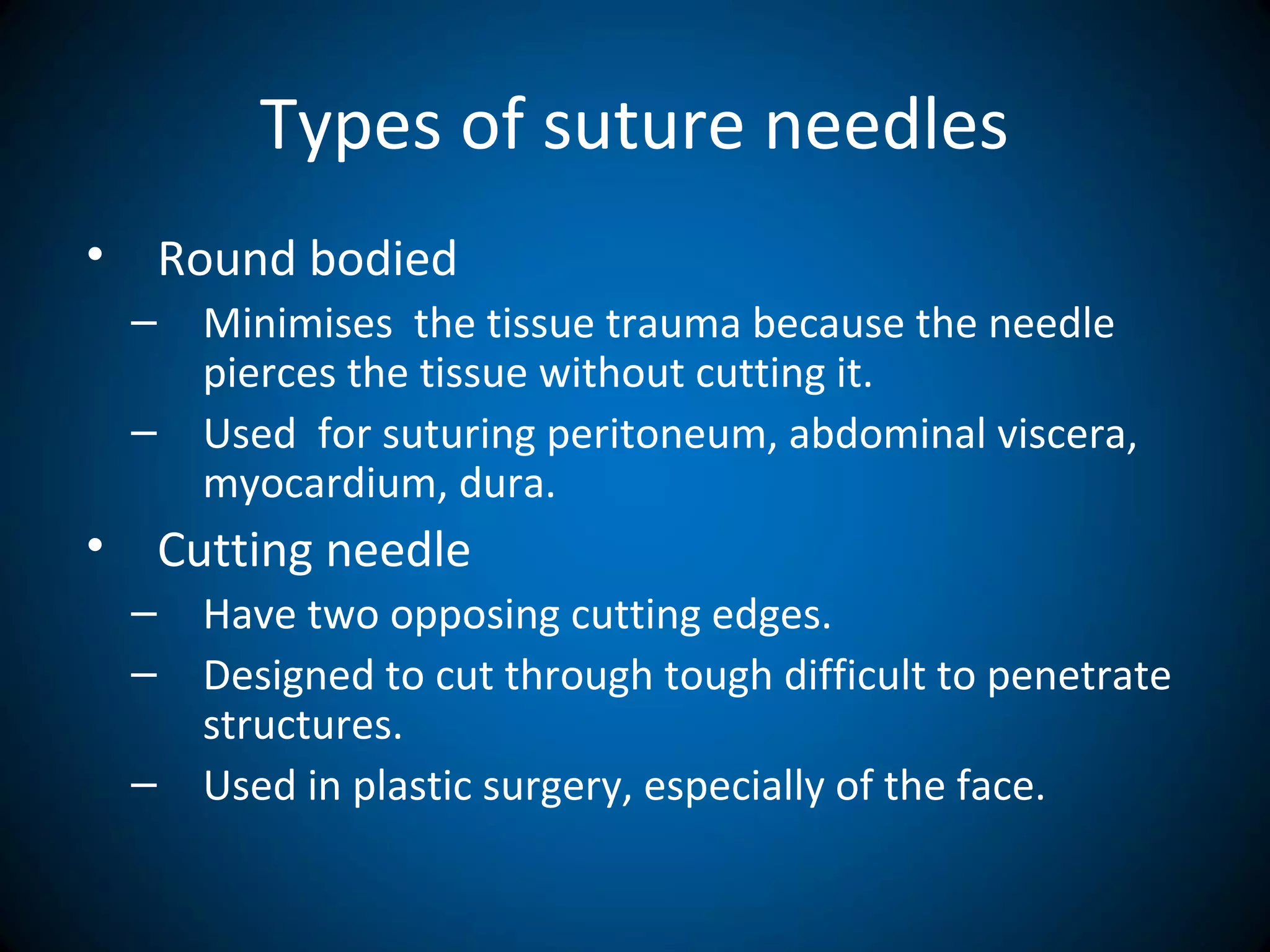
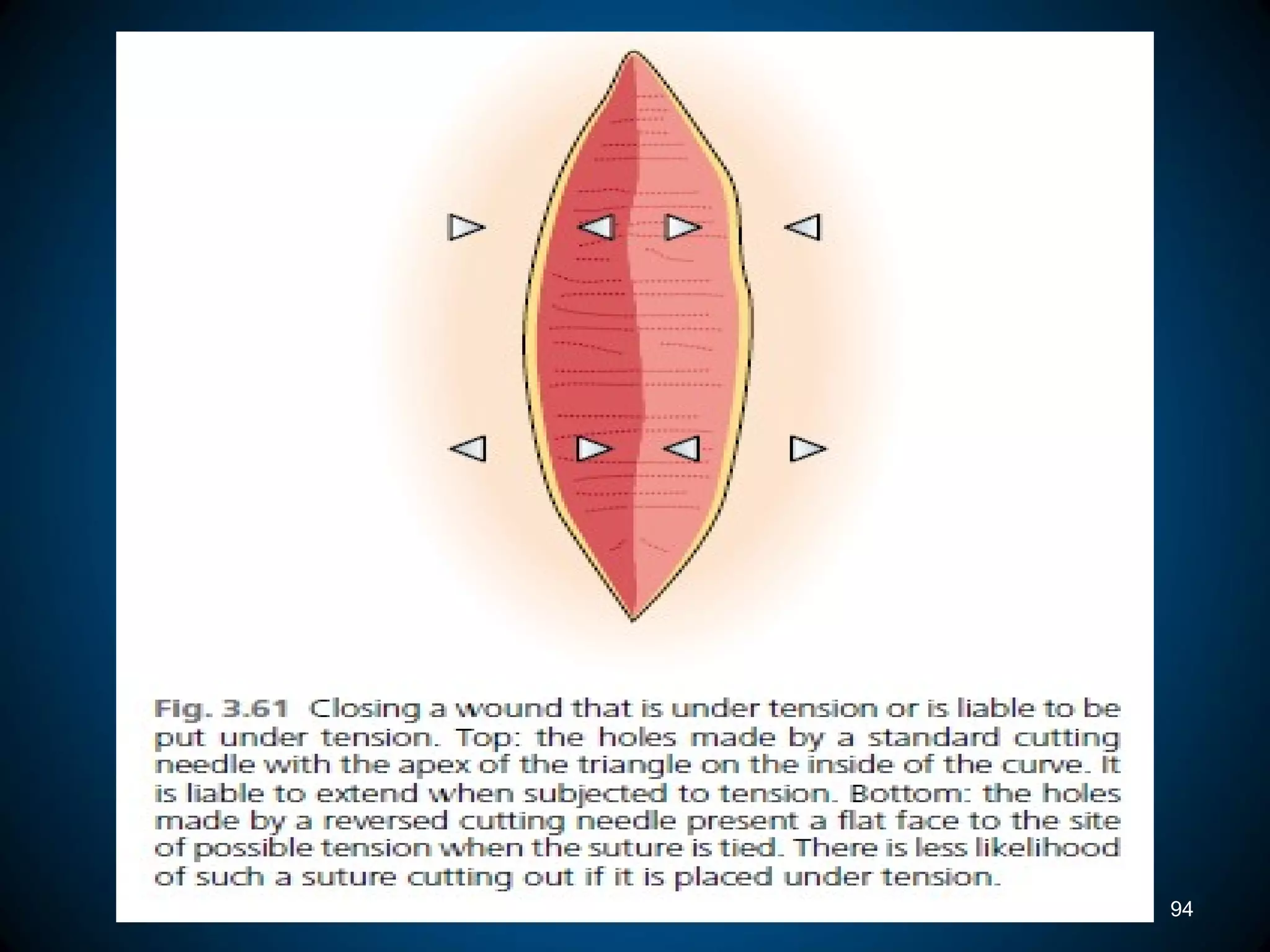
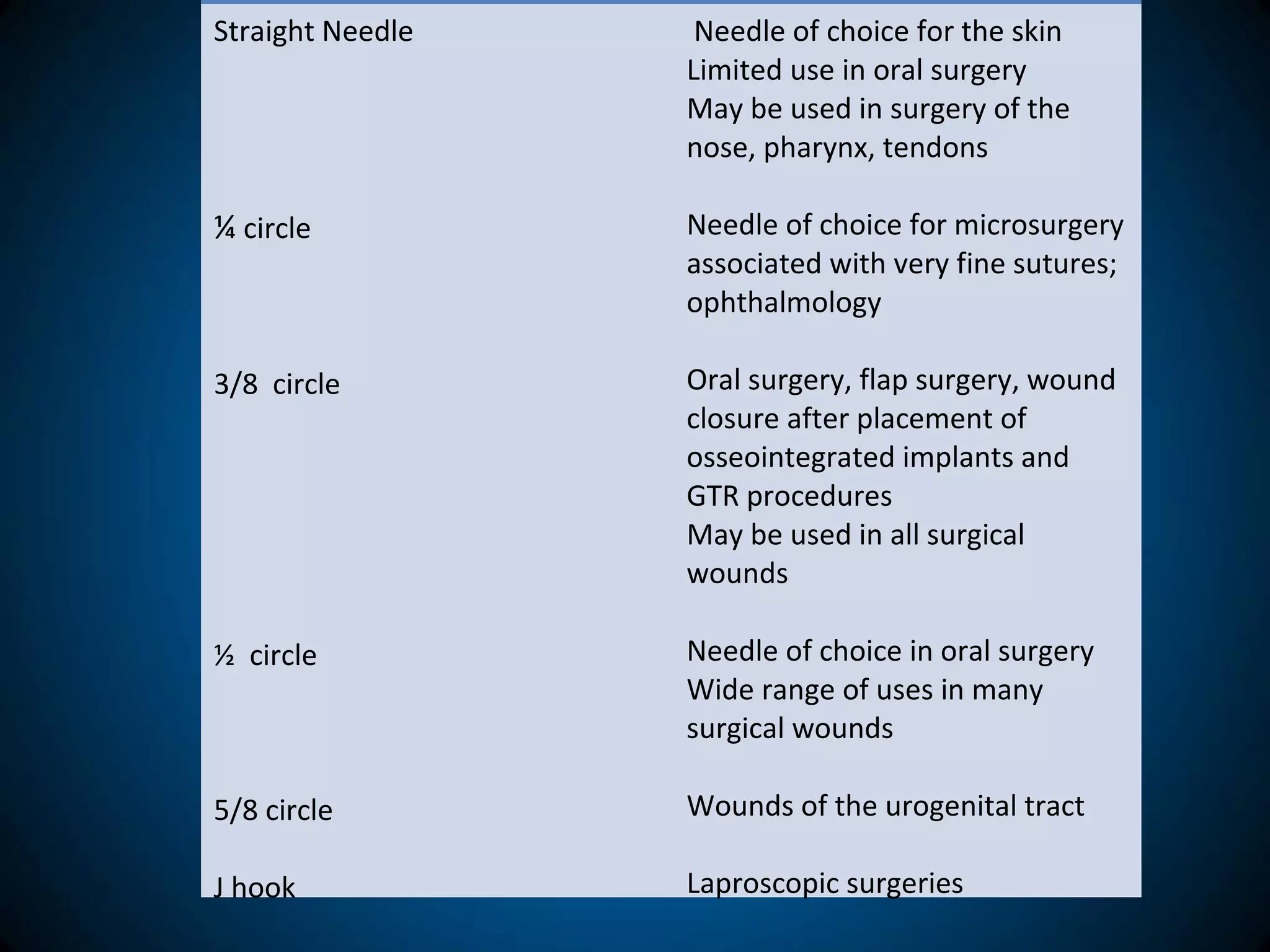
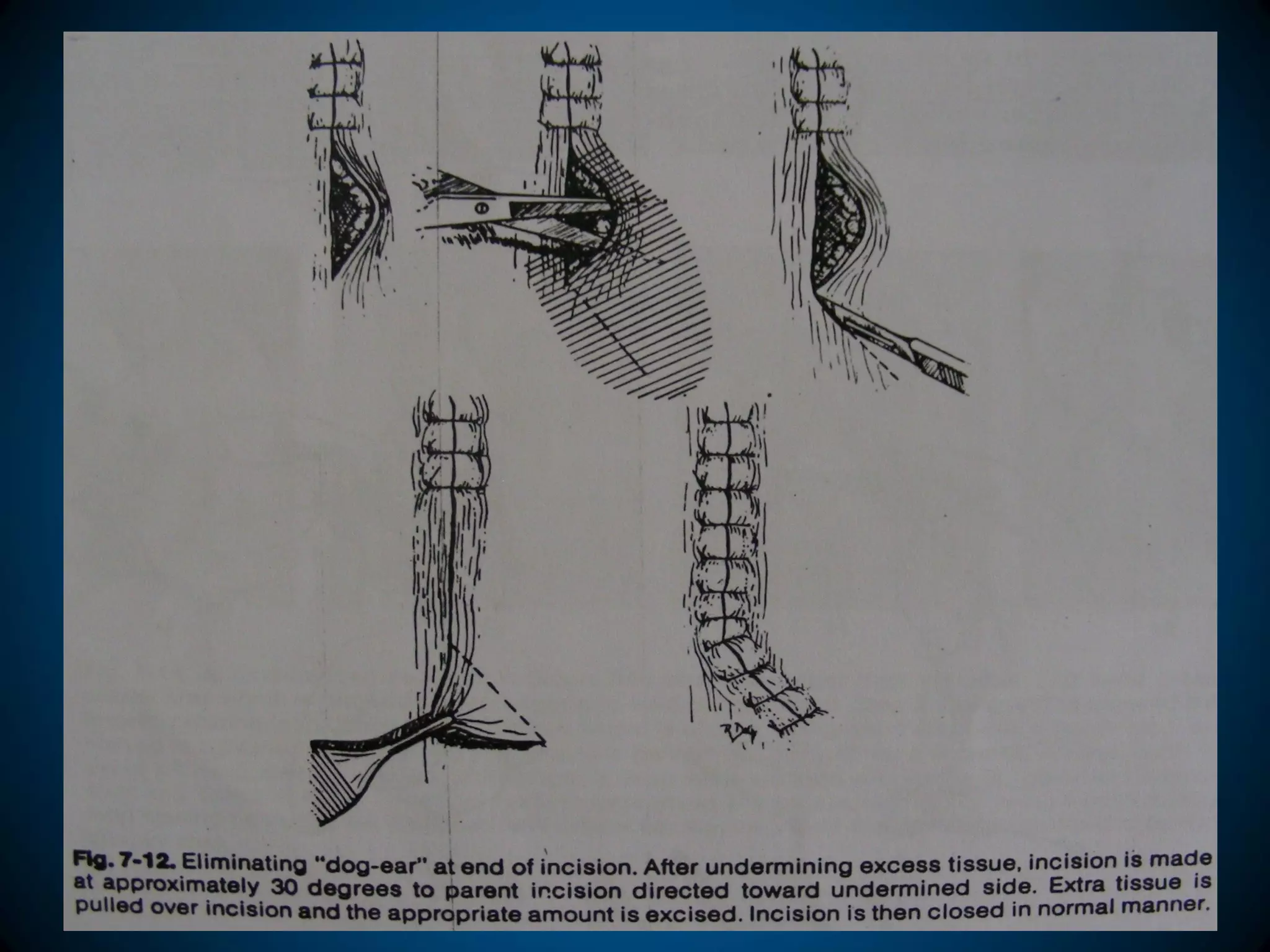
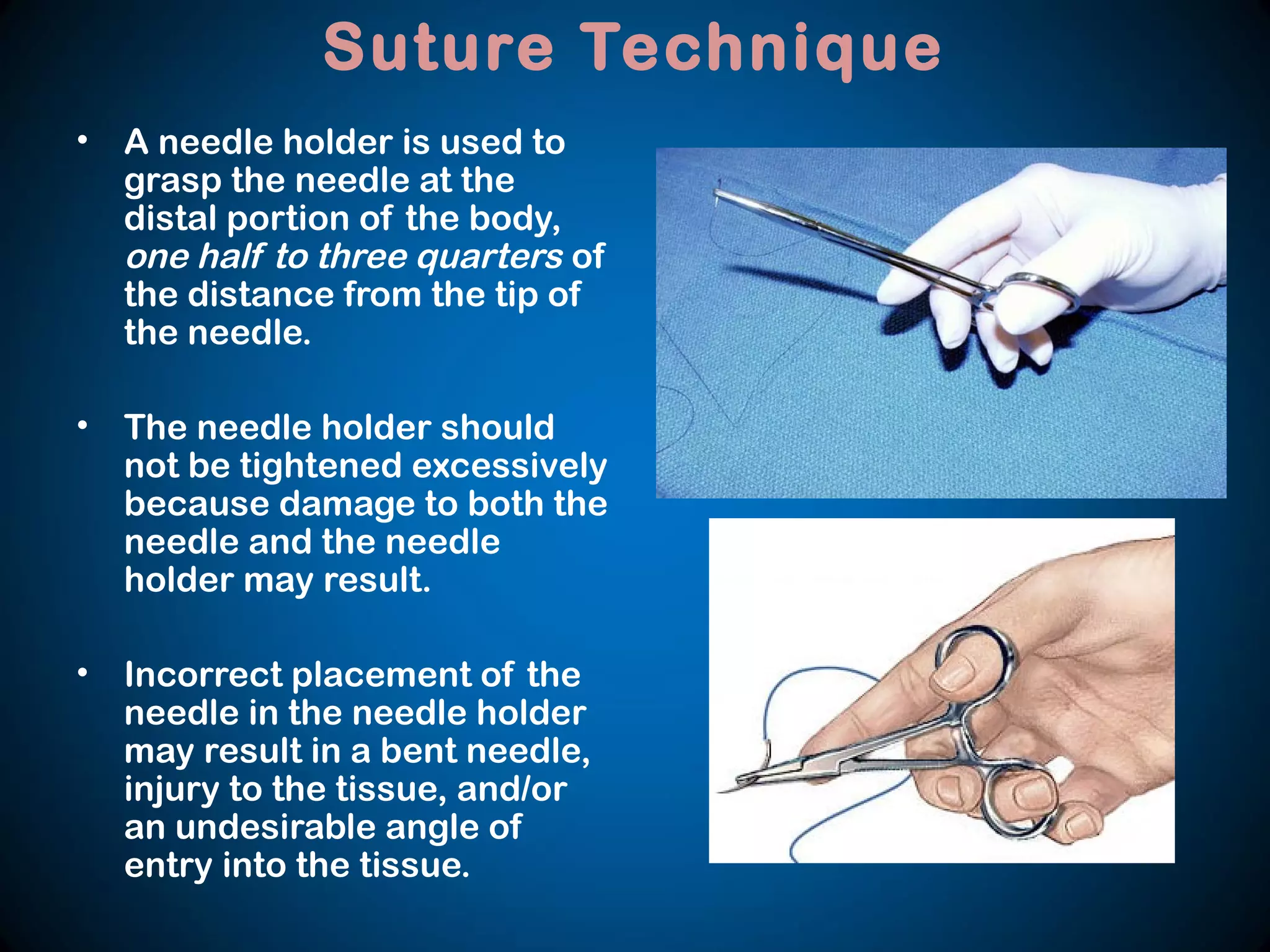
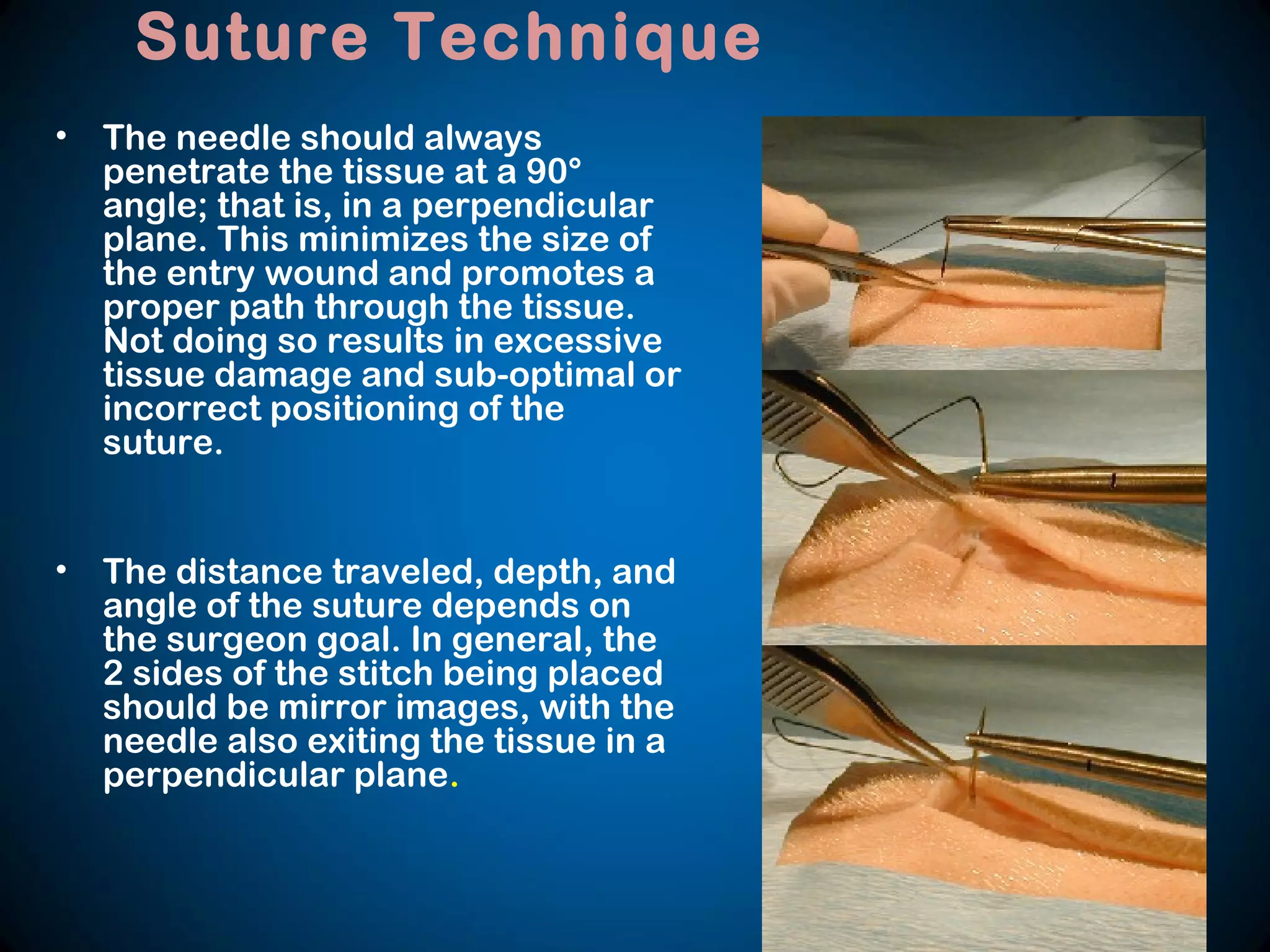
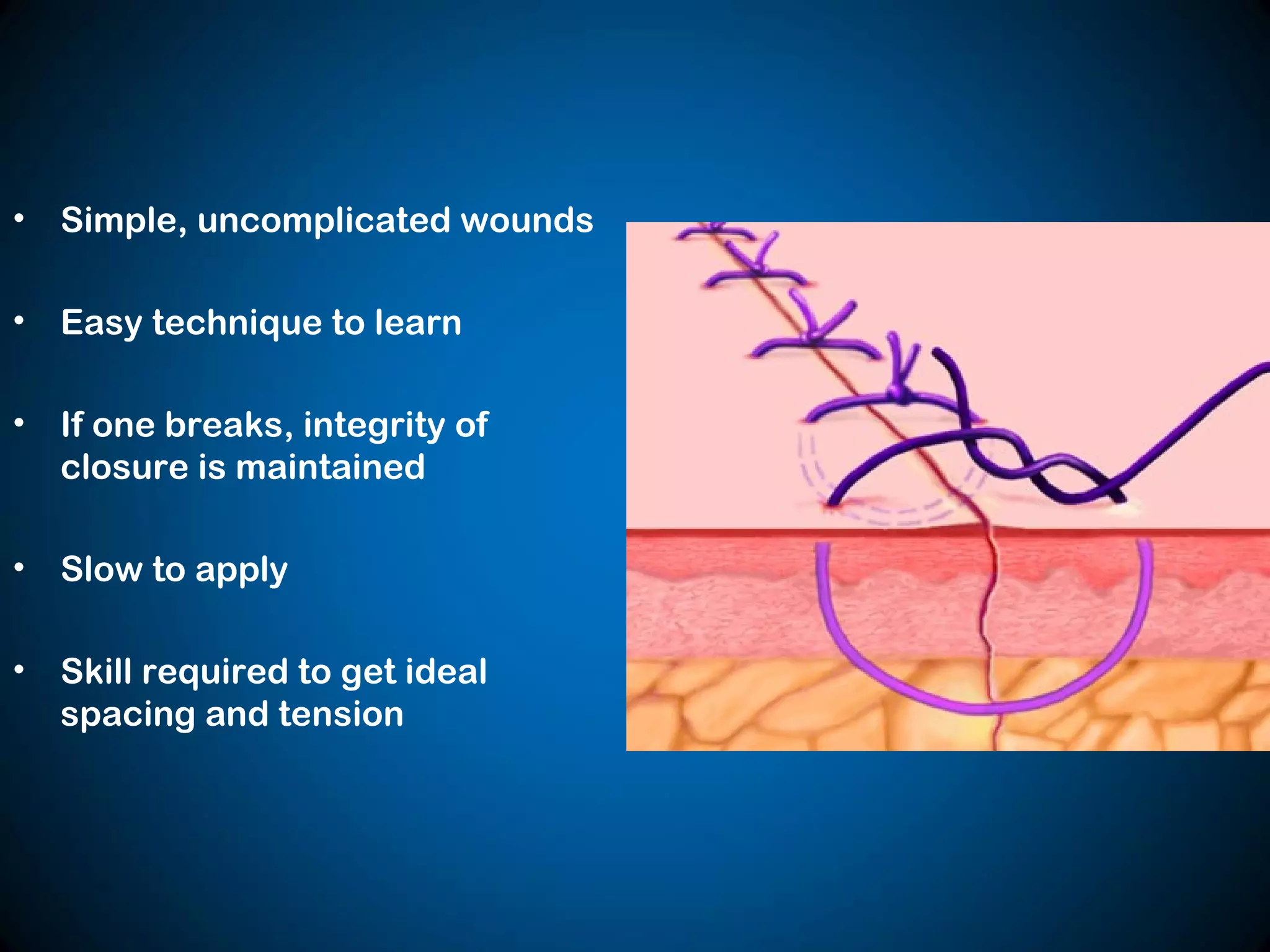
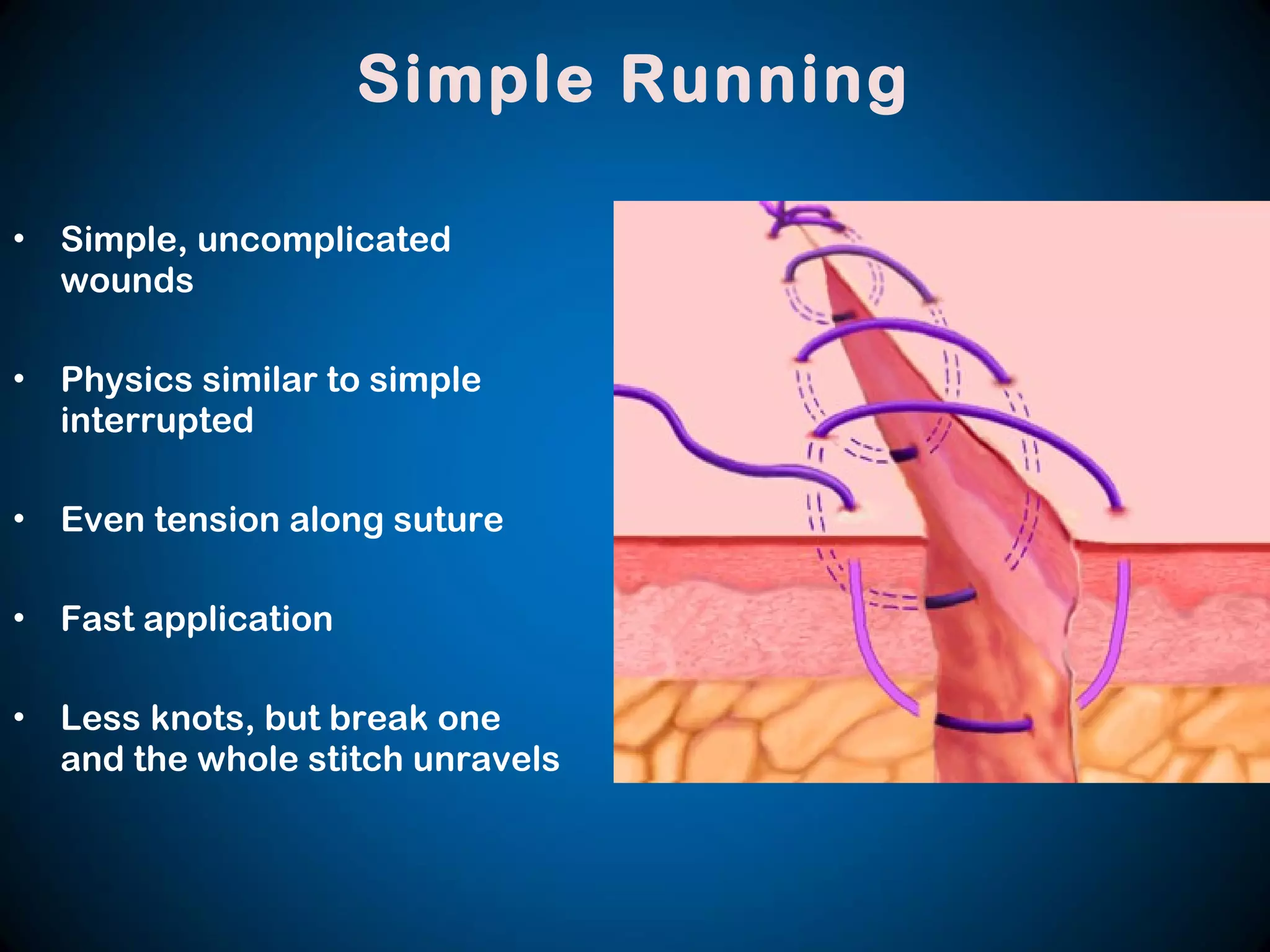
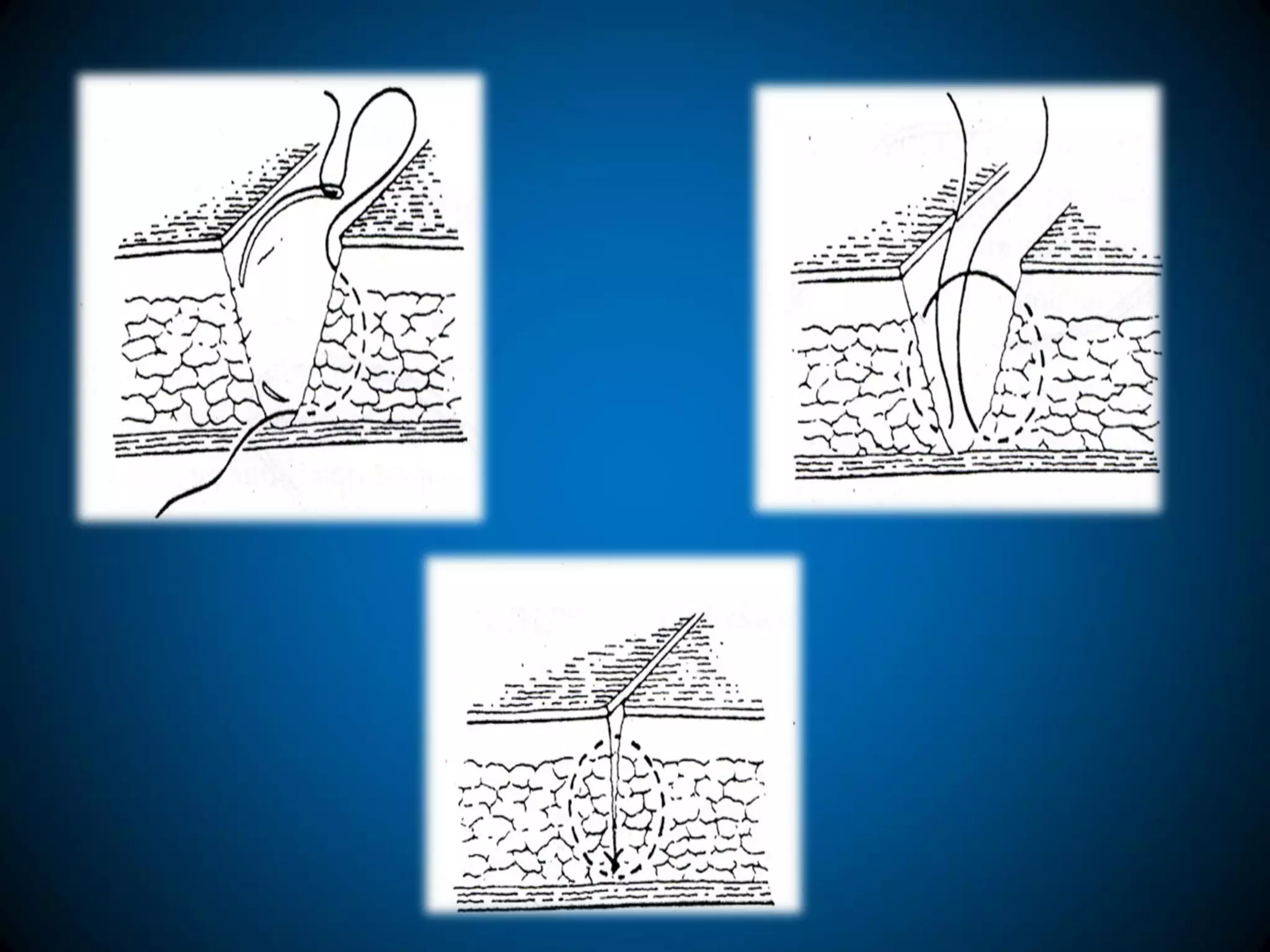
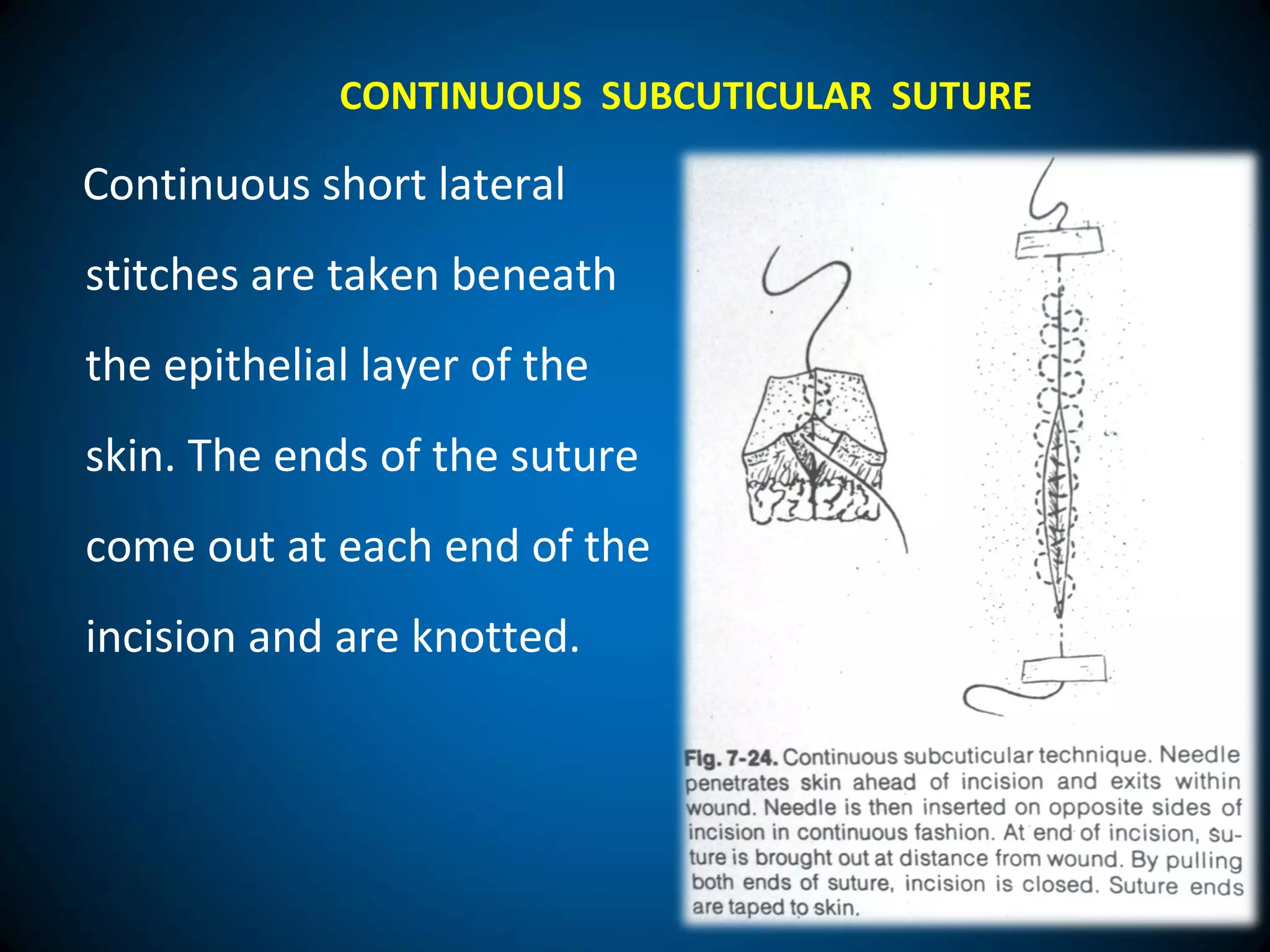
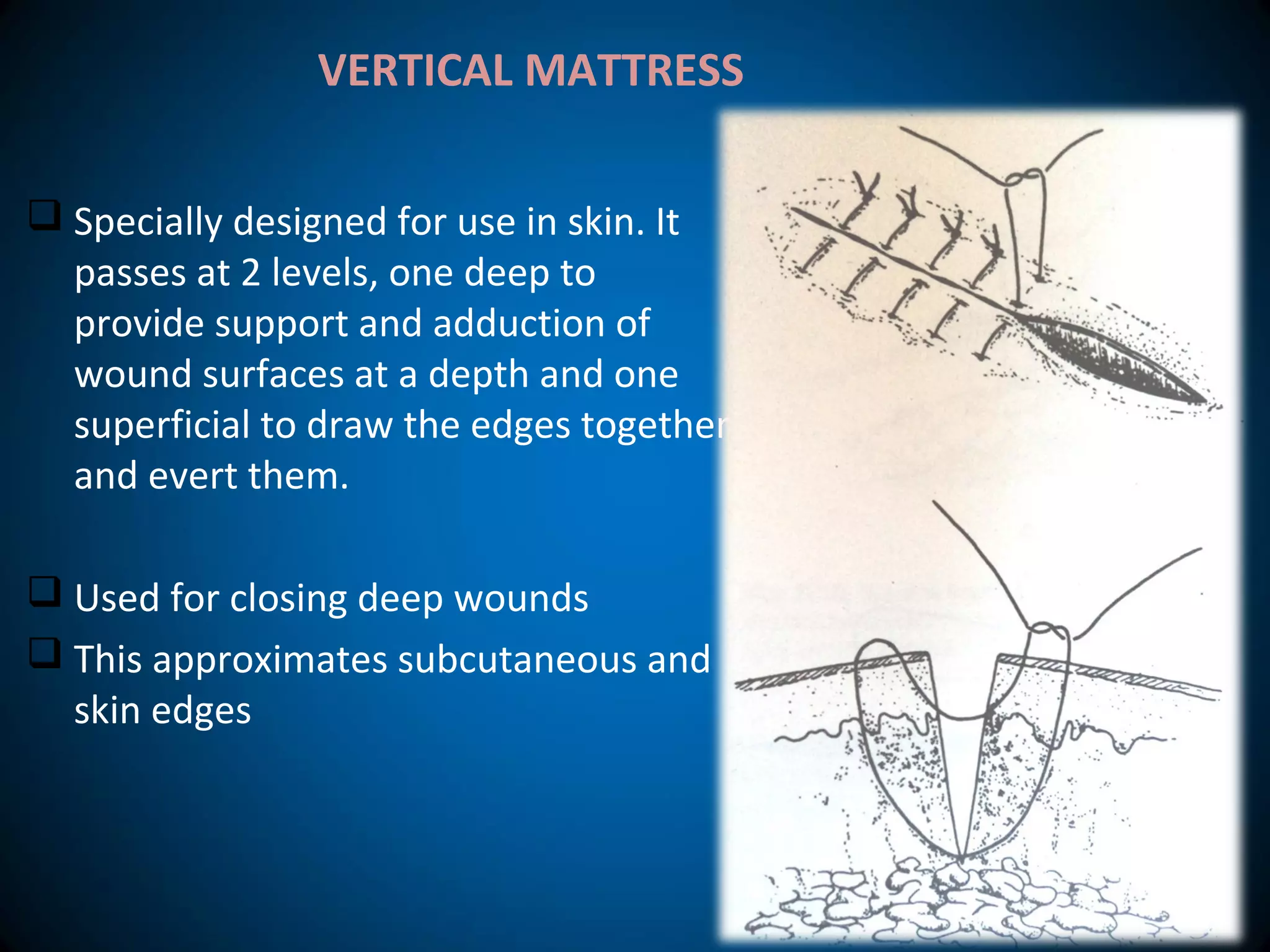
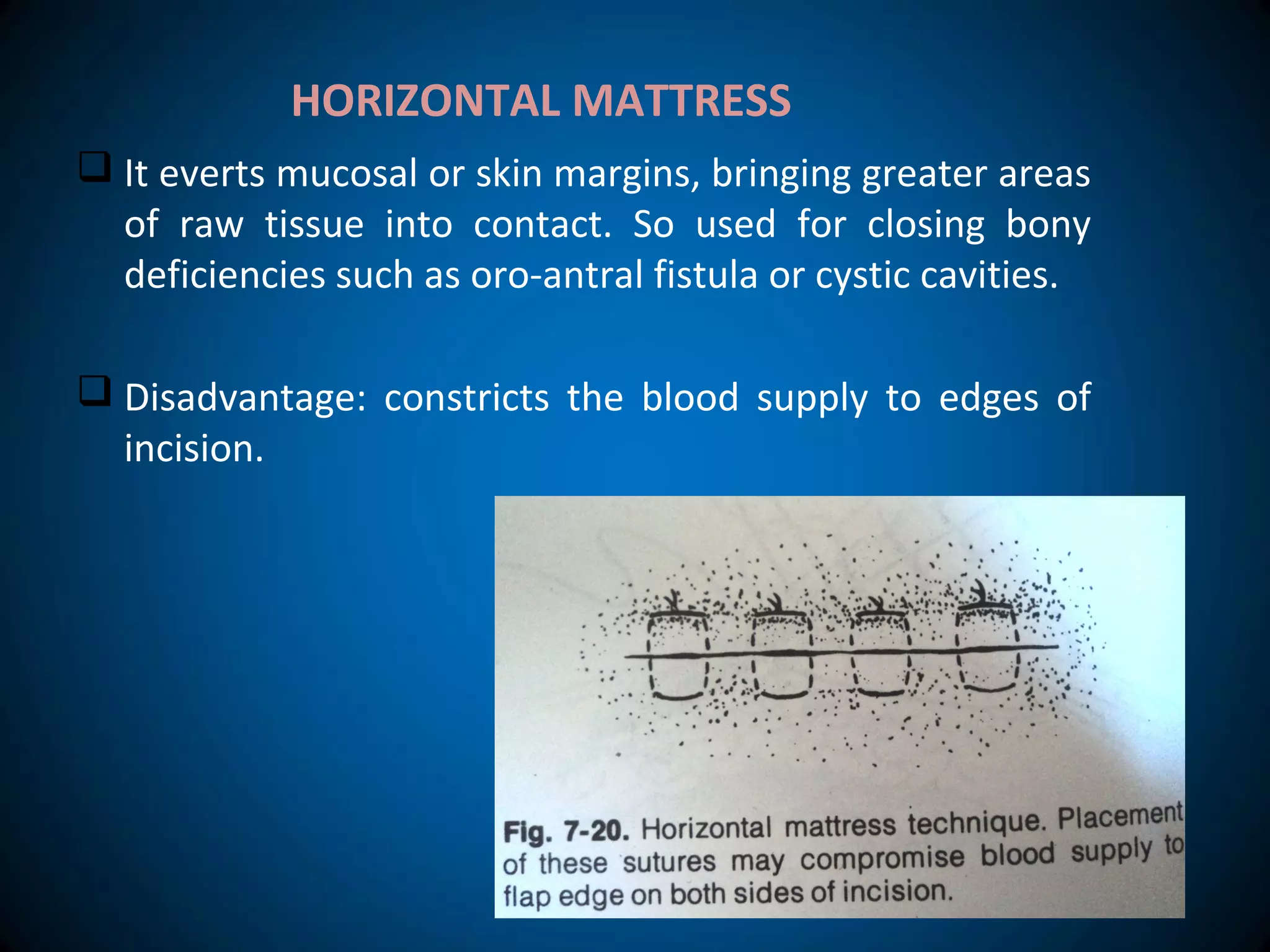
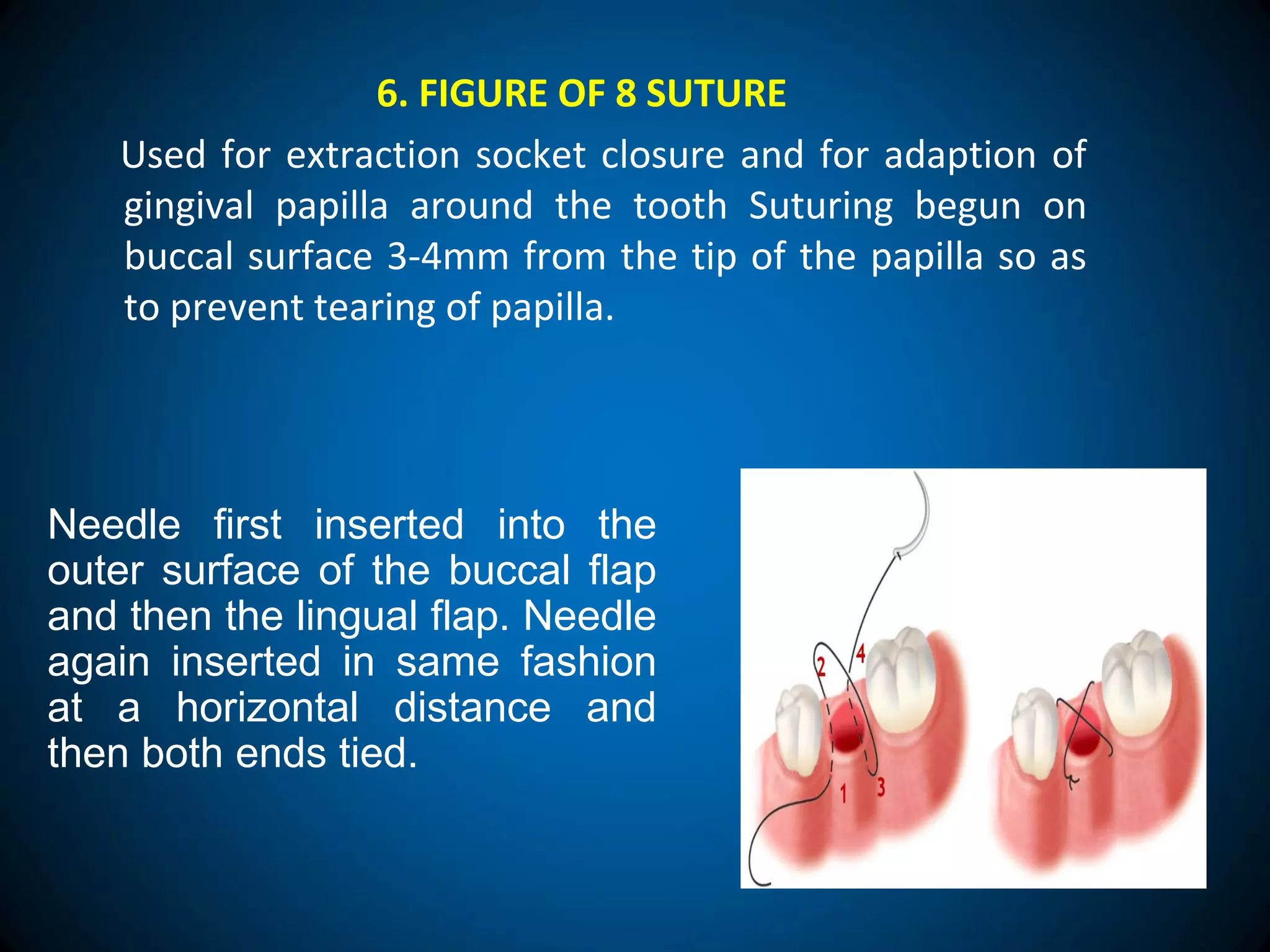
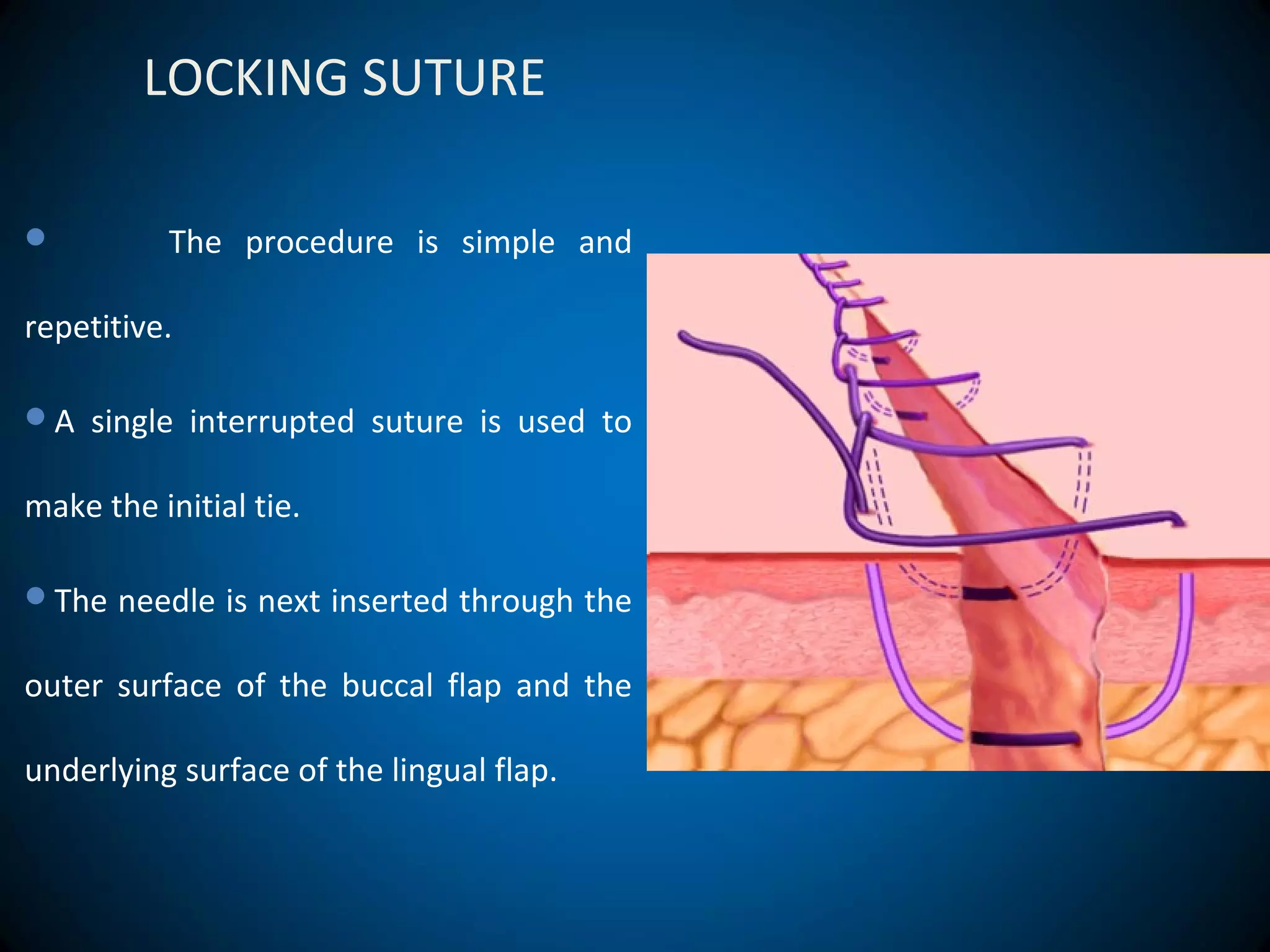
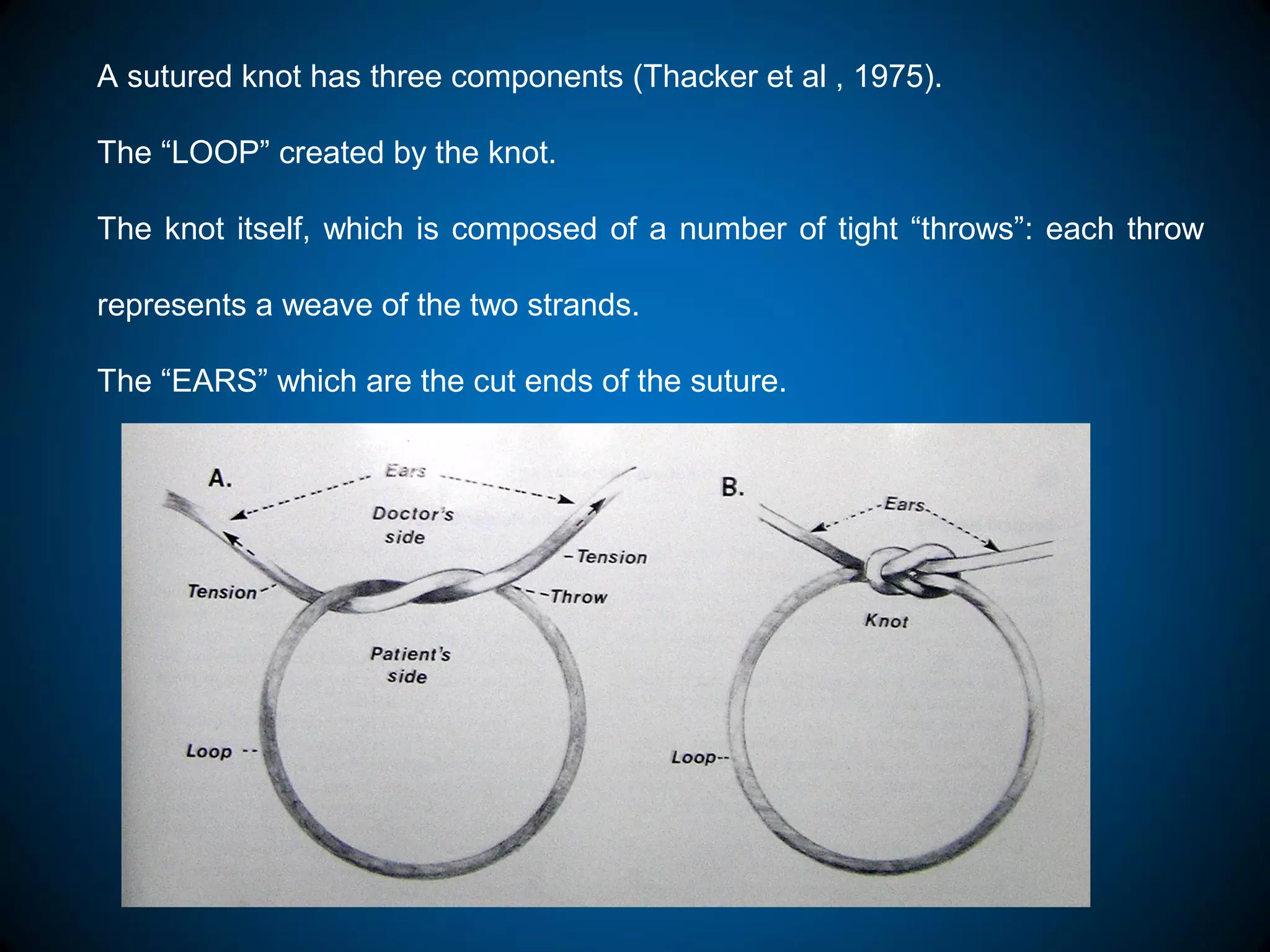
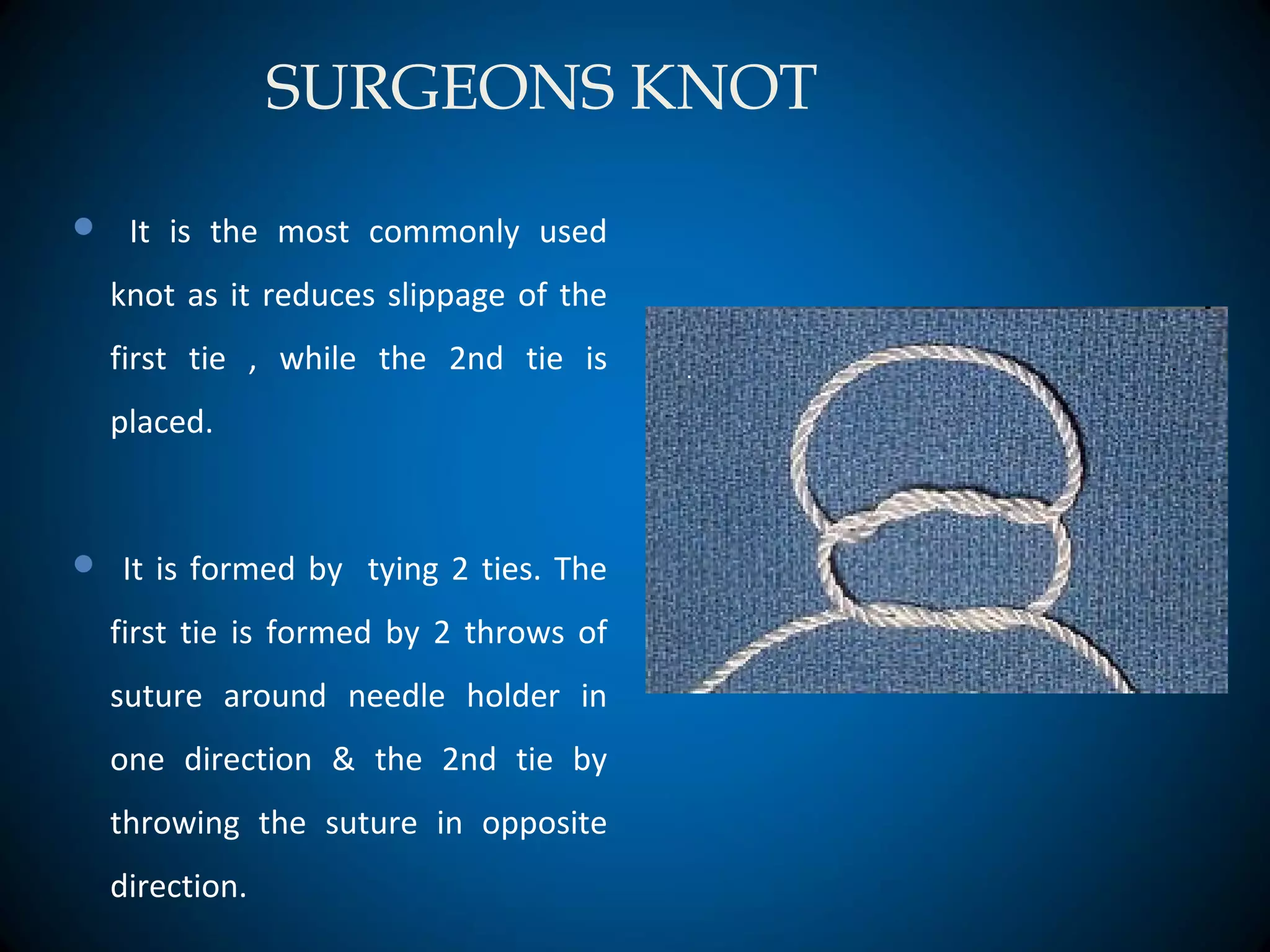
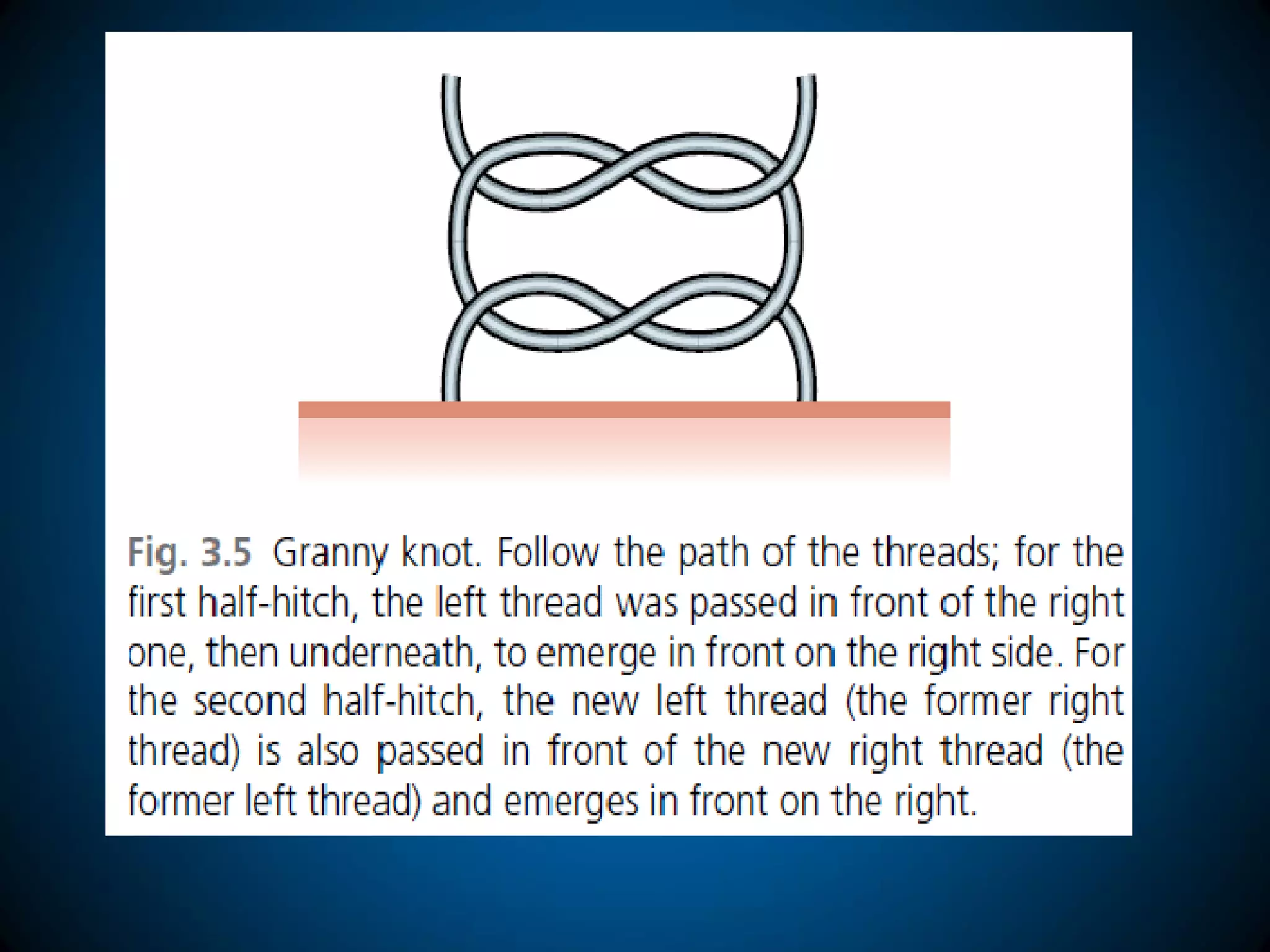
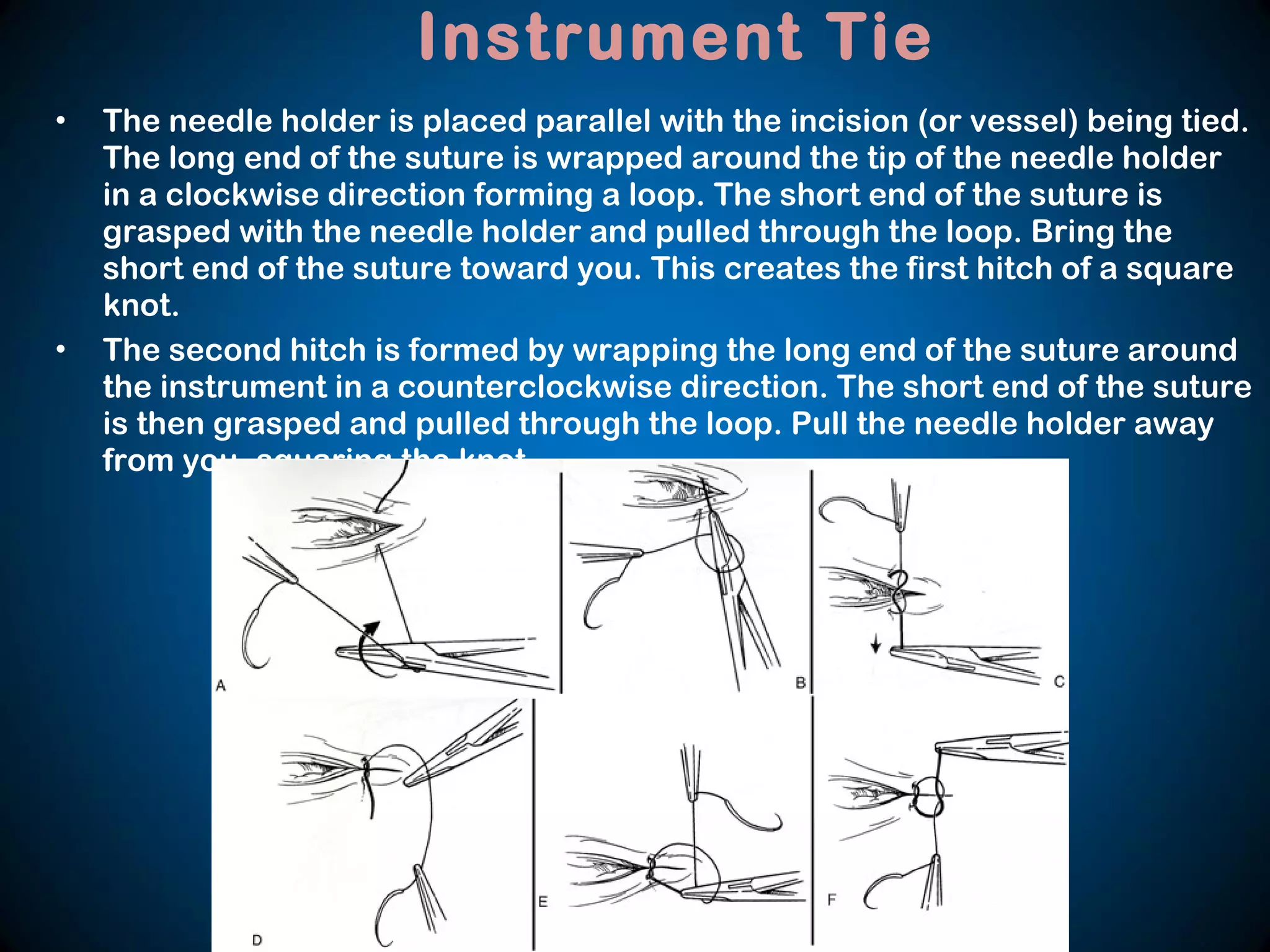
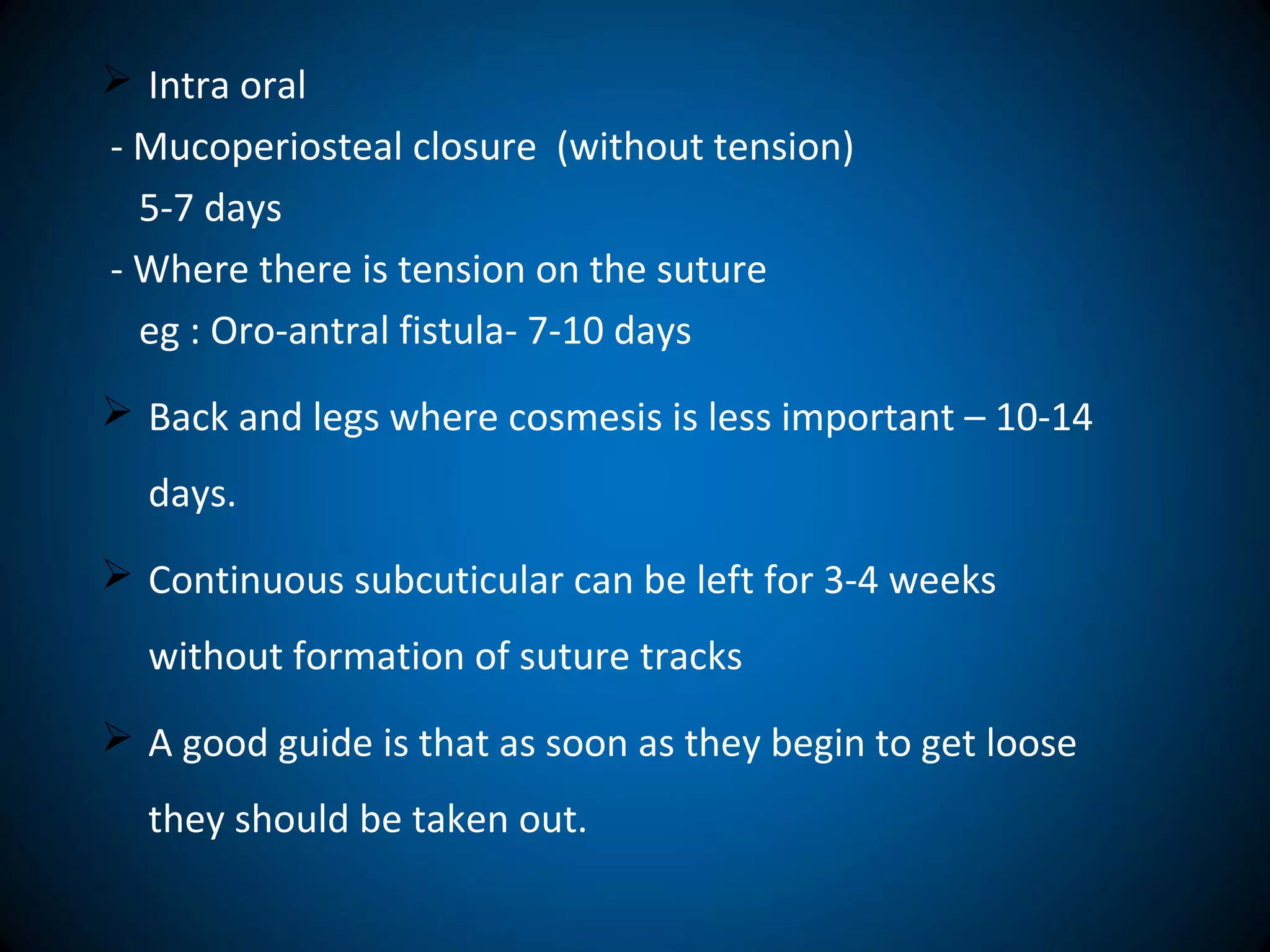
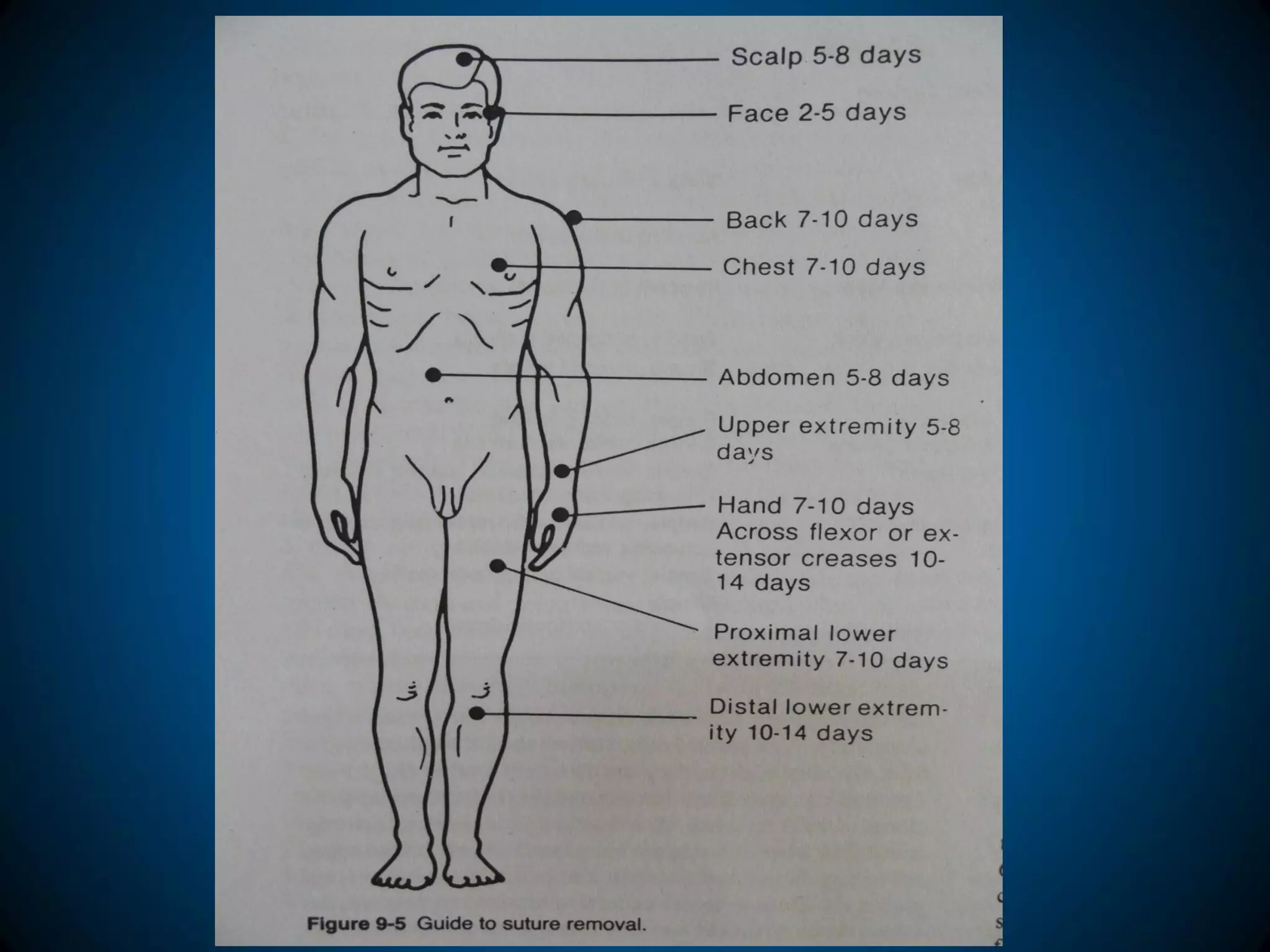
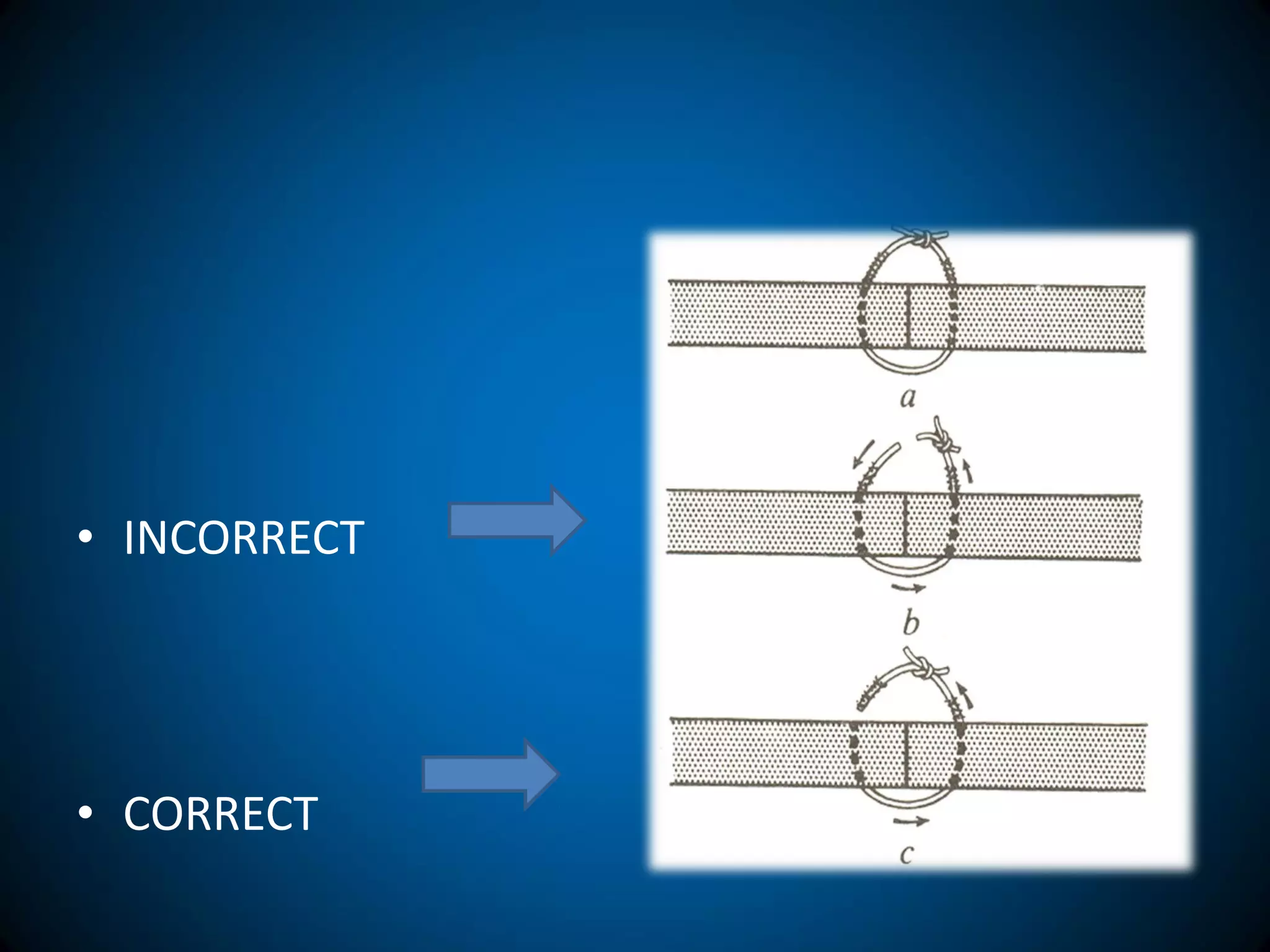
3. The principles of suturing, different suturing techniques, and knot tying are outlined in the document.