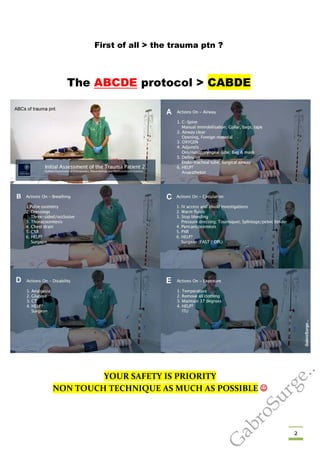
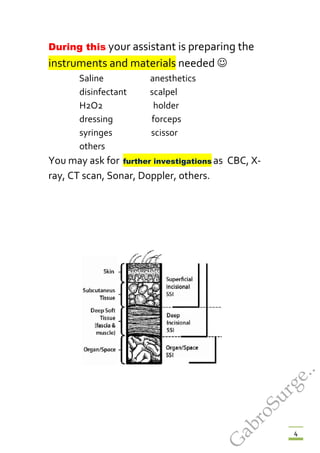
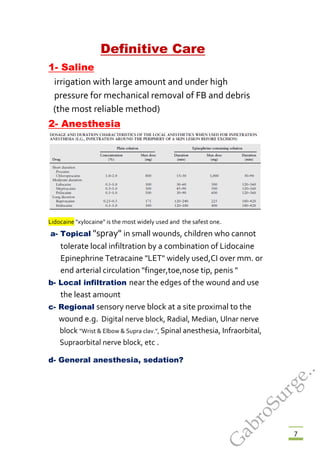
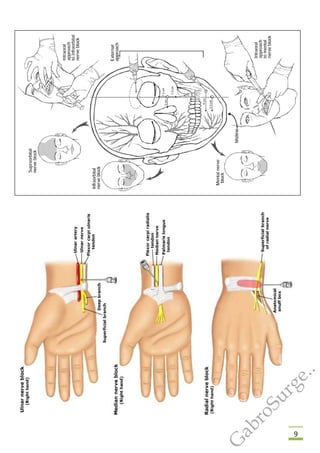
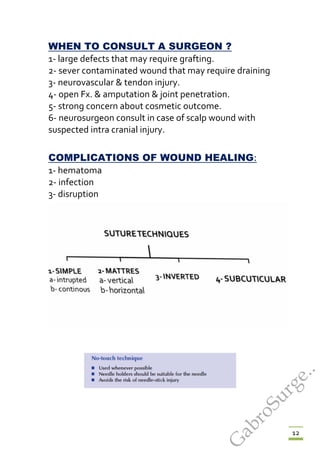
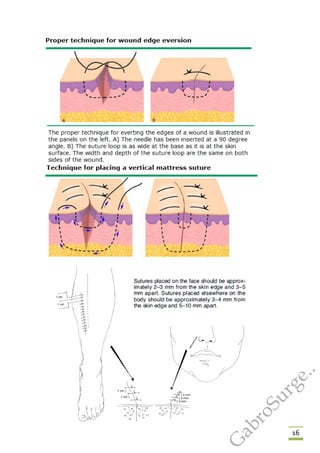
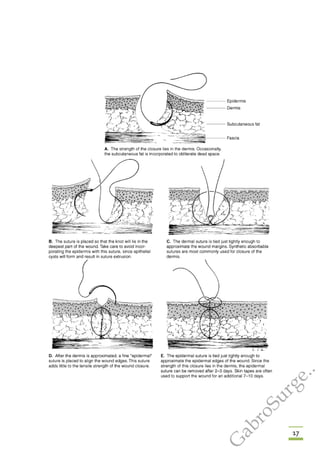
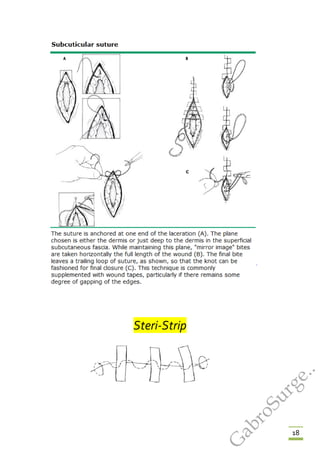
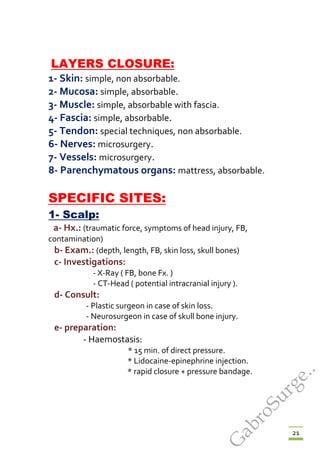
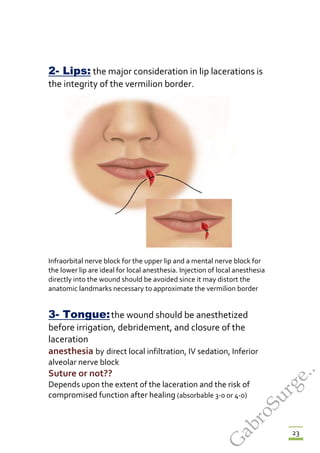
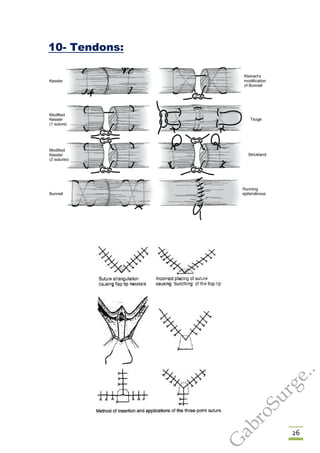
The document provides guidance on basic wound management. It outlines the ABCDE protocol for initially assessing a trauma patient and controlling bleeding. It then describes in detail how to clean, debride, close and provide post-operative care for different types of wounds, including through suturing techniques. Specific wound locations like the face, eyes and joints are addressed. Proper wound closure and follow-up are emphasized to prevent complications and support proper healing.