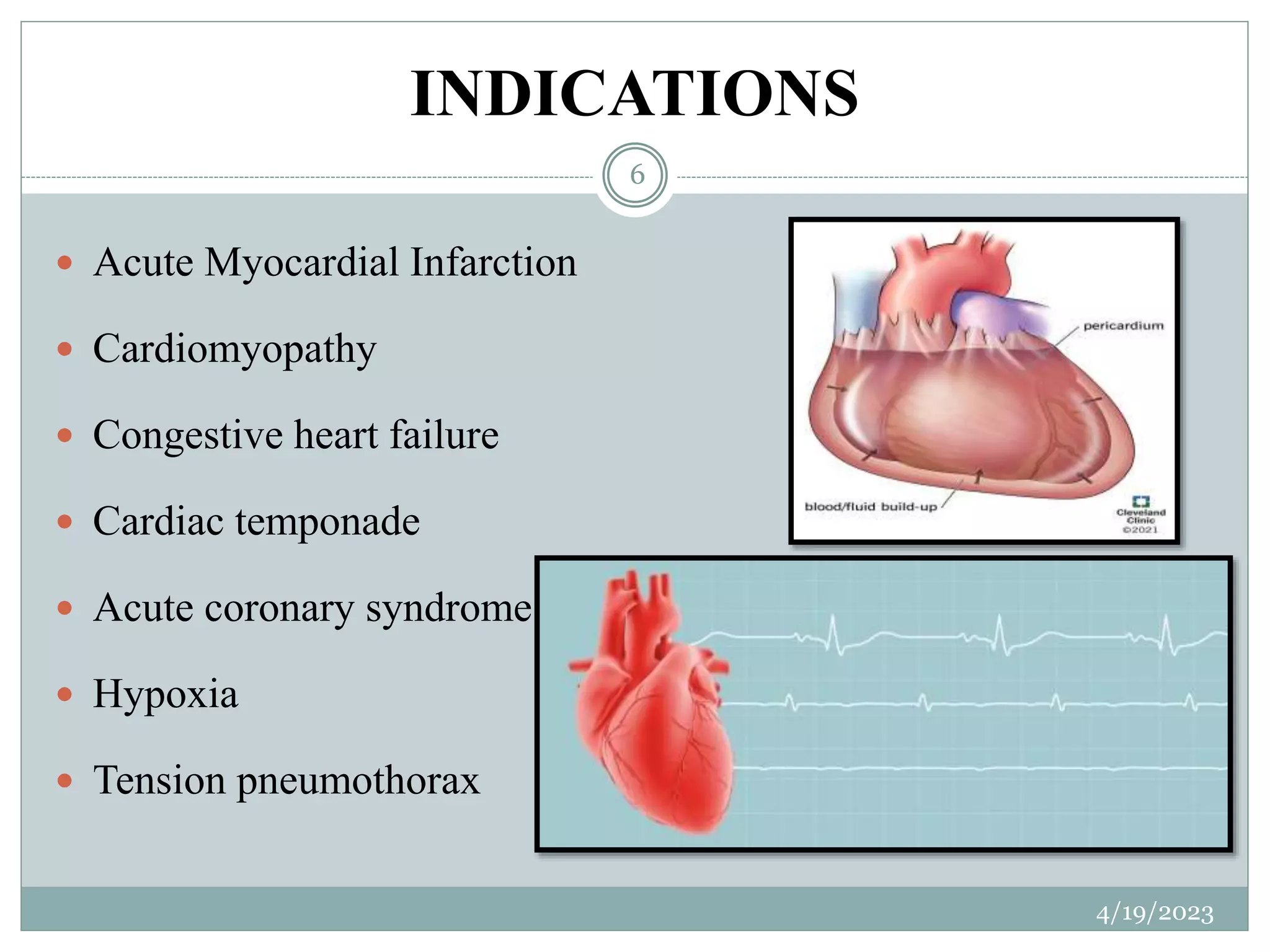
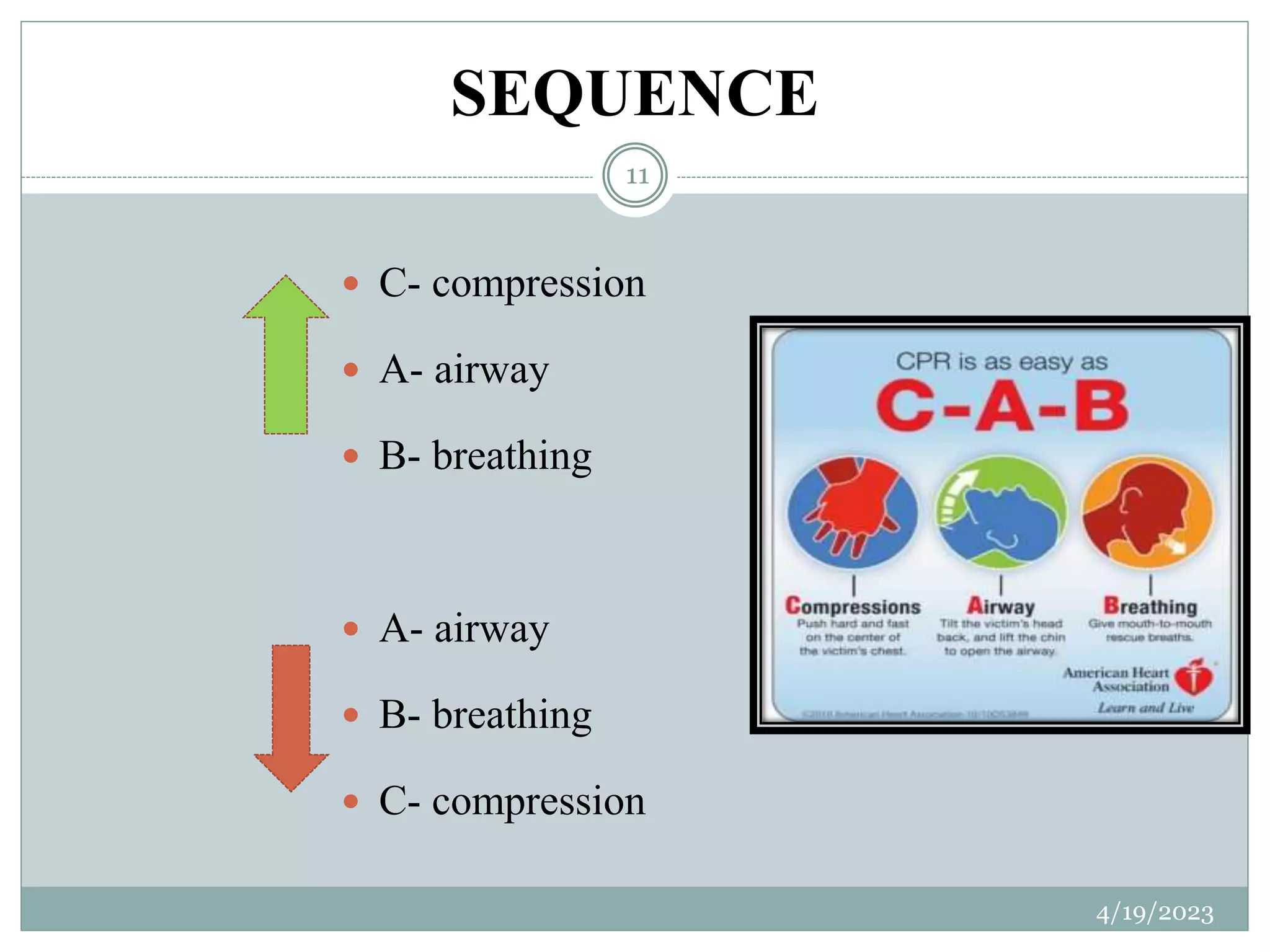
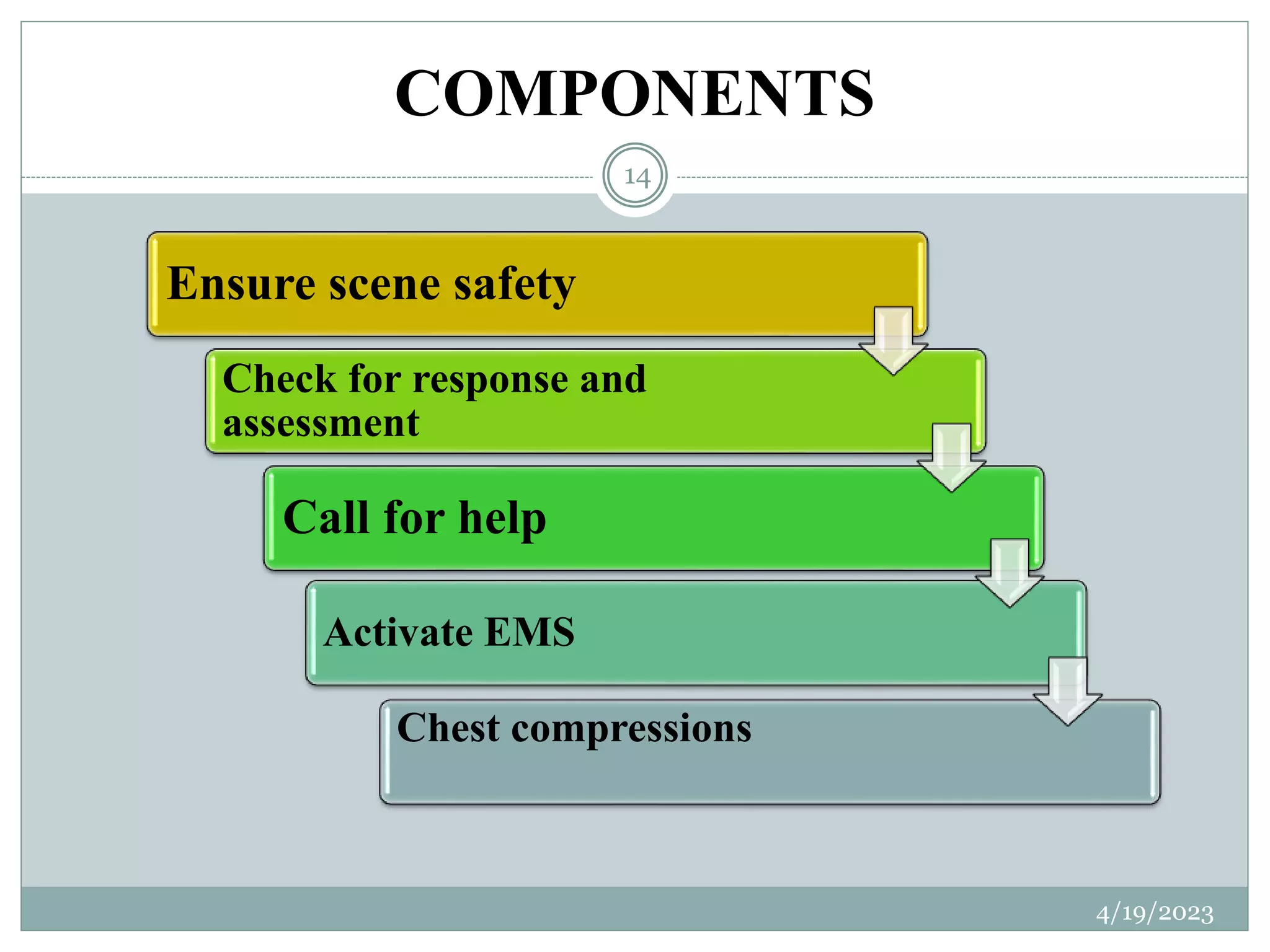
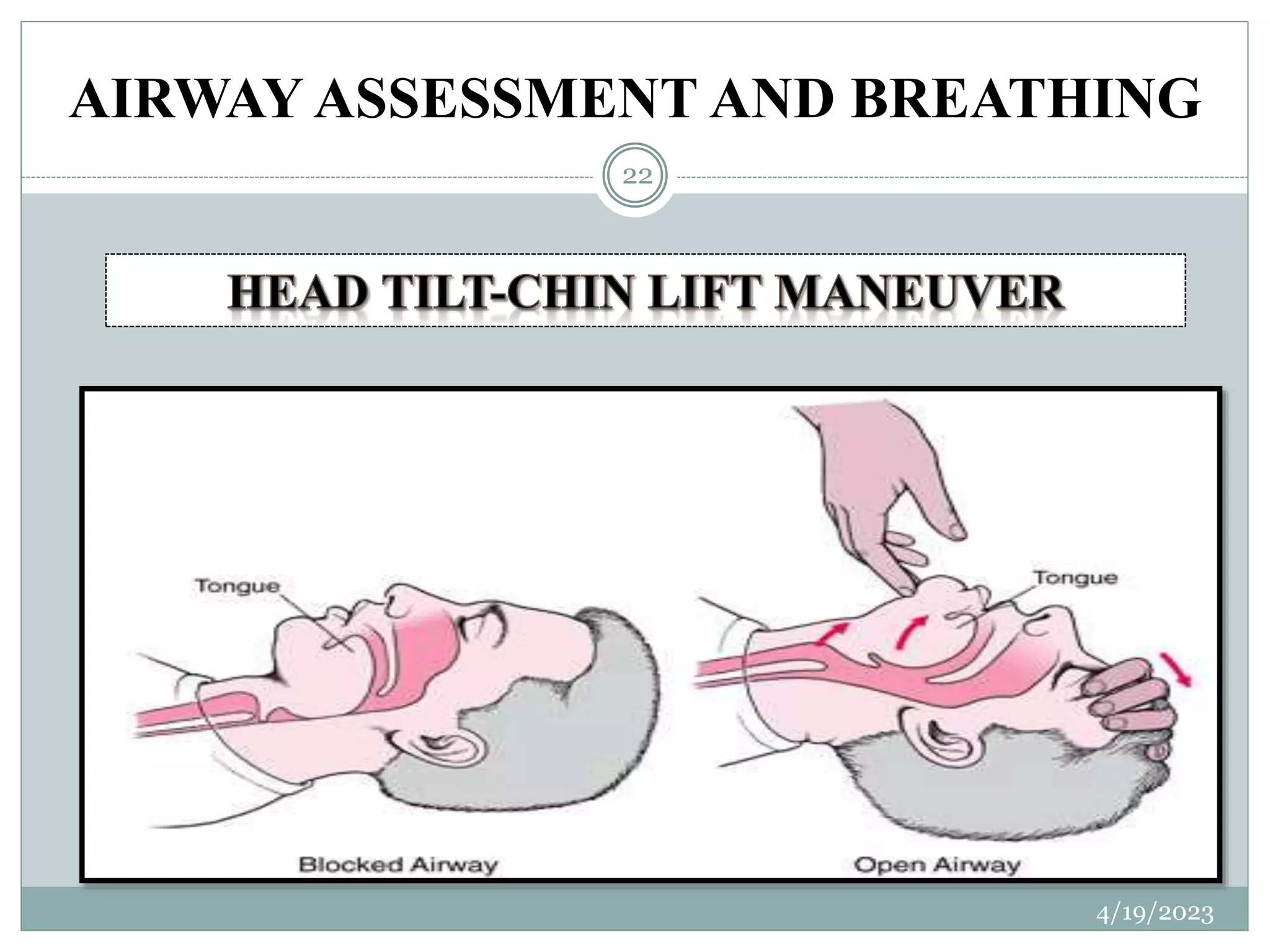
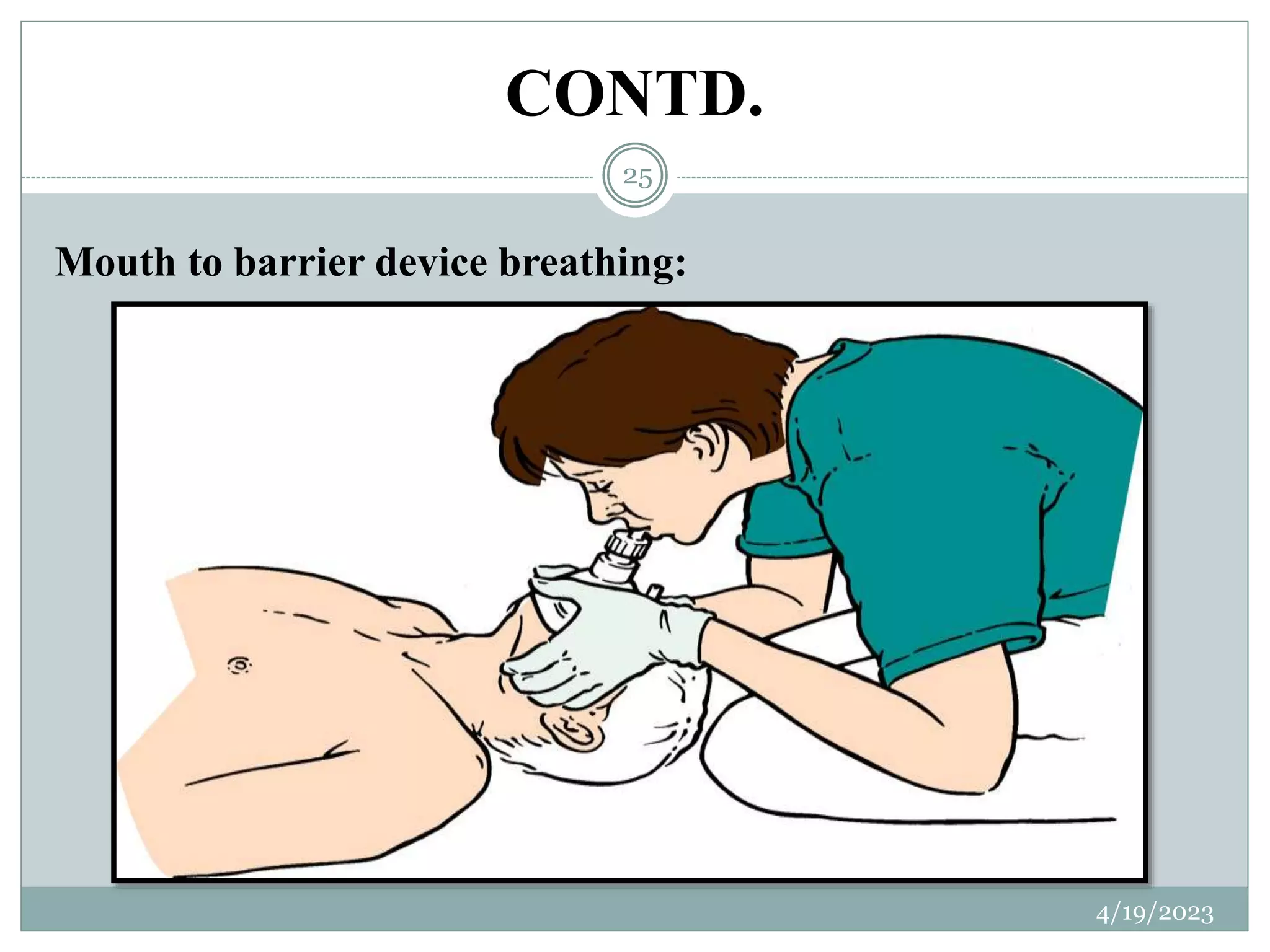
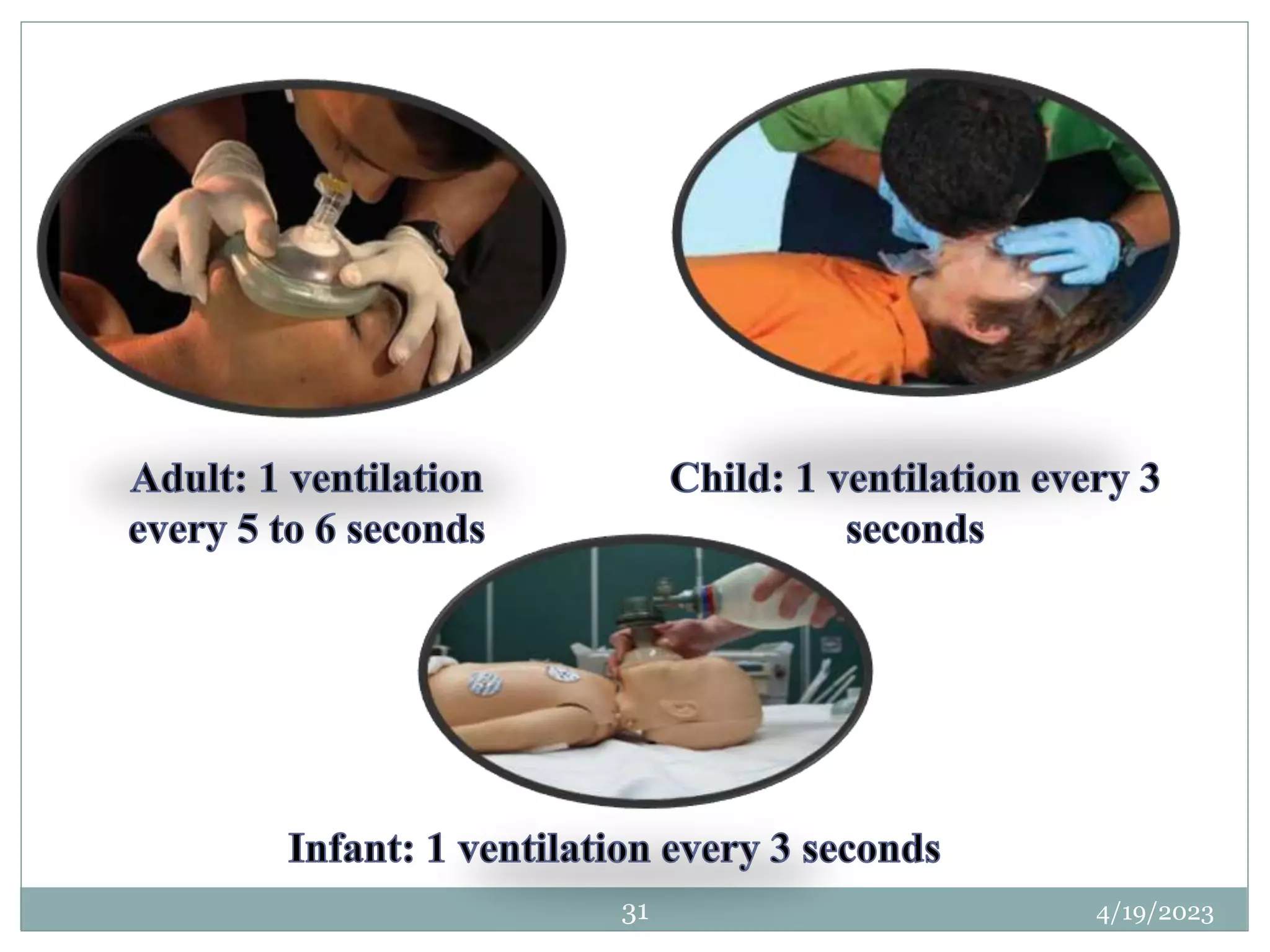
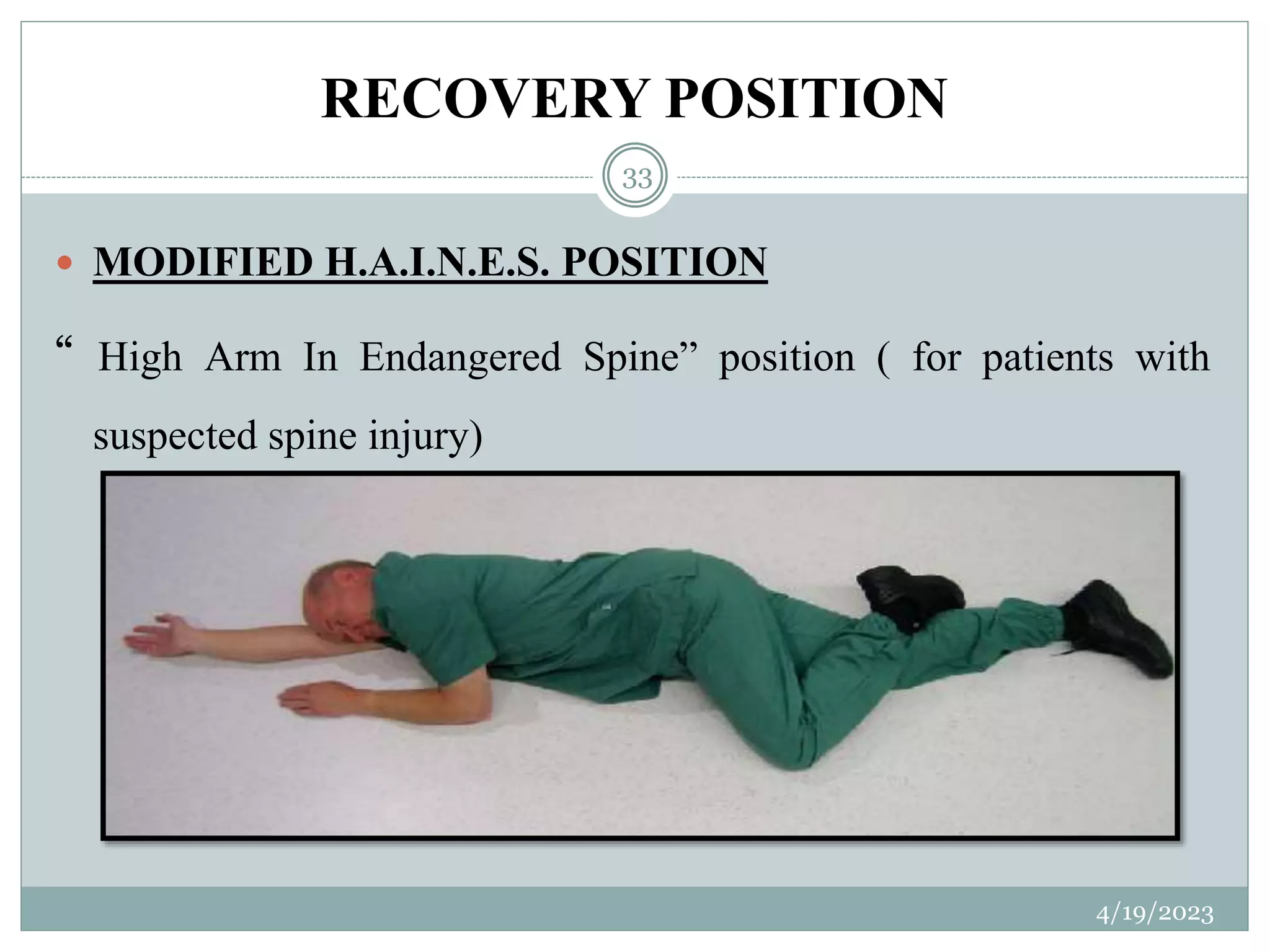
The document provides an overview of cardiopulmonary resuscitation (CPR). It discusses the history of CPR from early attempts at resuscitation in the 18th century to modern CPR guidelines established in 2000. It defines CPR as an emergency procedure that uses chest compressions and artificial ventilation to manually restore blood circulation and breathing for someone in cardiac arrest. The document also outlines the purposes, indications, techniques, types (BLS, ACLS), medications, and importance of high-quality CPR performance to maximize survival from cardiac arrest.