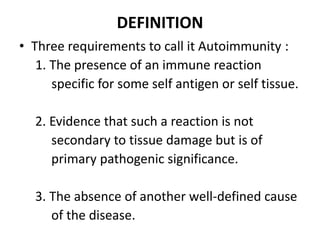
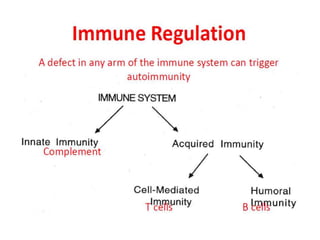
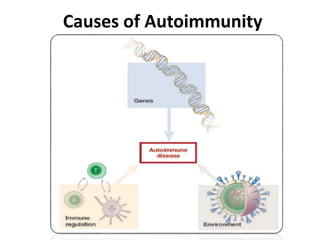
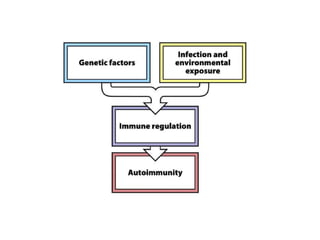
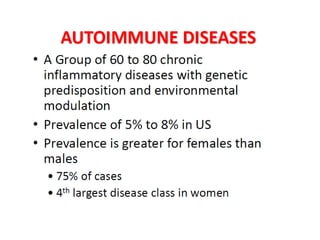
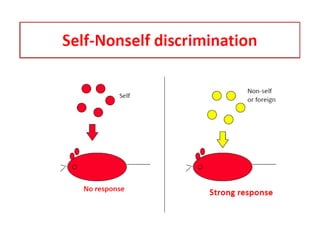
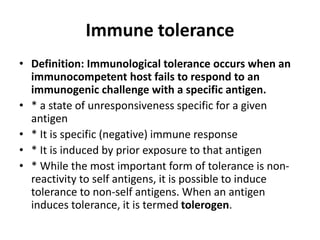
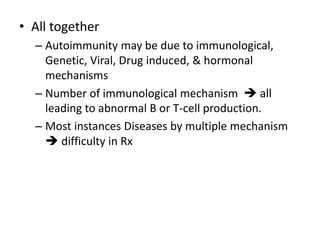
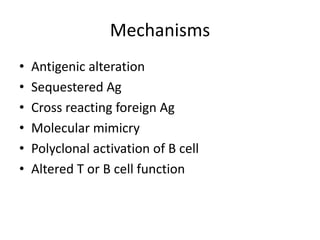
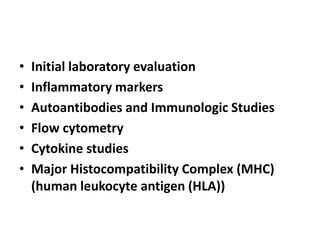
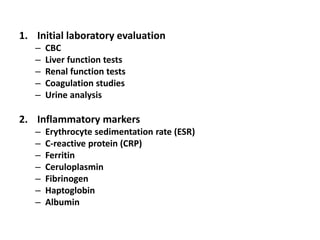
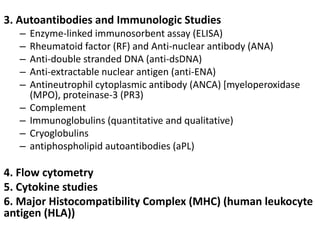
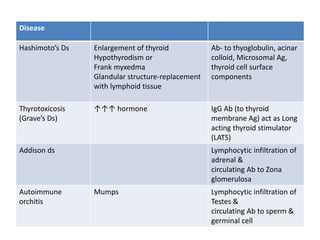
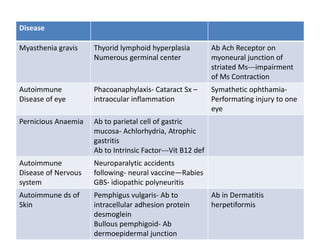
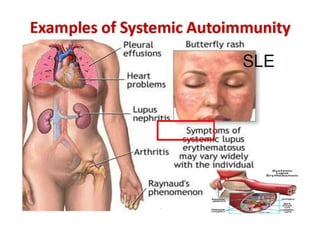
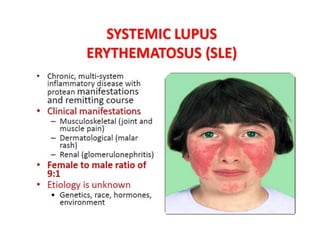
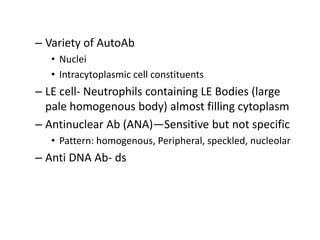
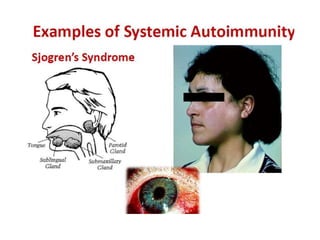
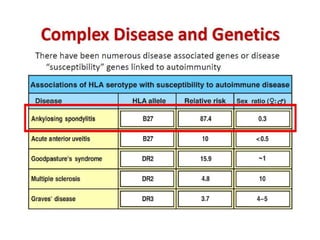
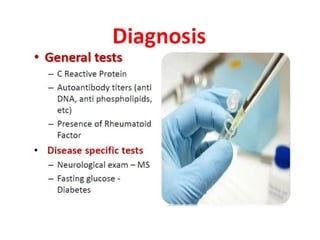
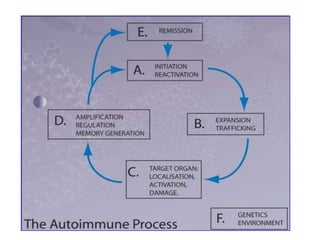
Autoimmunity disorders occur when the immune system mounts an attack against the body's own tissues and organs. They are difficult to diagnose due to nonspecific initial symptoms, fluctuating symptoms, and the potential for multiple autoimmune conditions. Diagnostic methods include initial laboratory tests of inflammatory markers and autoantibodies, immunological studies, flow cytometry to analyze immune cells, cytokine studies, and examination of major histocompatibility complex genes associated with autoimmunity. A variety of autoantibodies against nuclear, cytoplasmic, and other cellular components can indicate autoimmune disease patterns and targets.