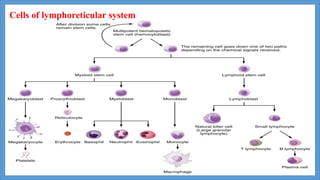
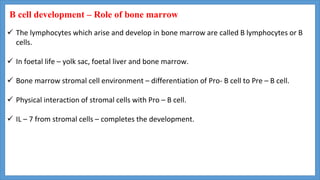
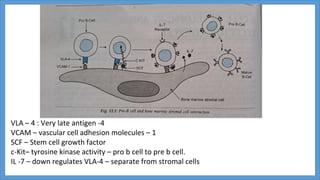
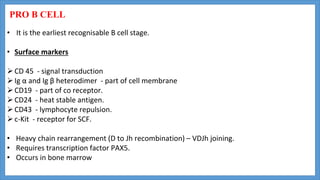
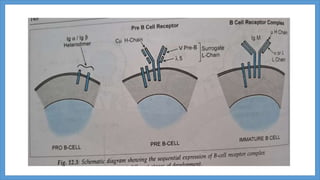
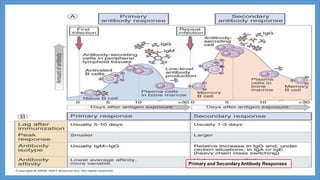
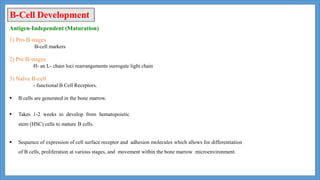
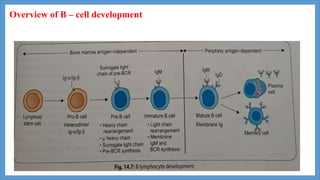
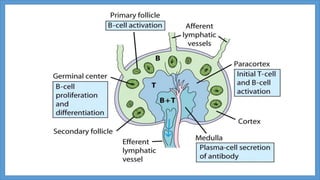
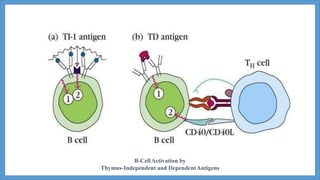
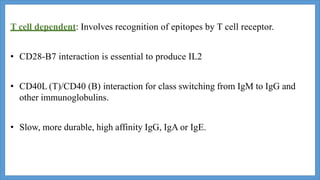
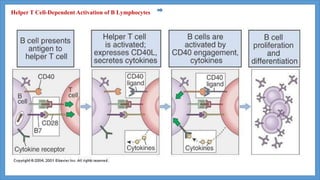
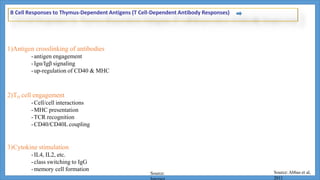
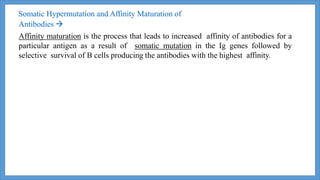
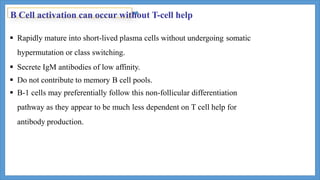
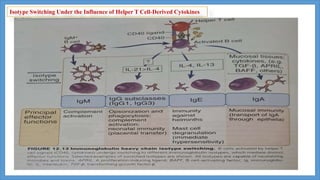
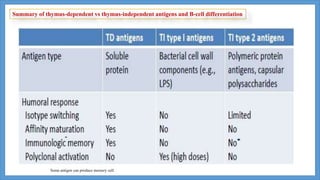
B-cell maturation begins with hematopoietic stem cells in the bone marrow, where they develop through pro-B cell, pre-B cell, and immature B cell stages. During this process, immunoglobulin genes undergo rearrangement and expression of B cell receptors occurs. Immature B cells then migrate to secondary lymphoid tissues to complete maturation. Mature B cells circulate and are activated by antigen to proliferate and differentiate into plasma cells or memory B cells through T cell dependent or independent pathways. T cell dependent activation induces affinity maturation, class switching, and generation of long-lived memory B cells.