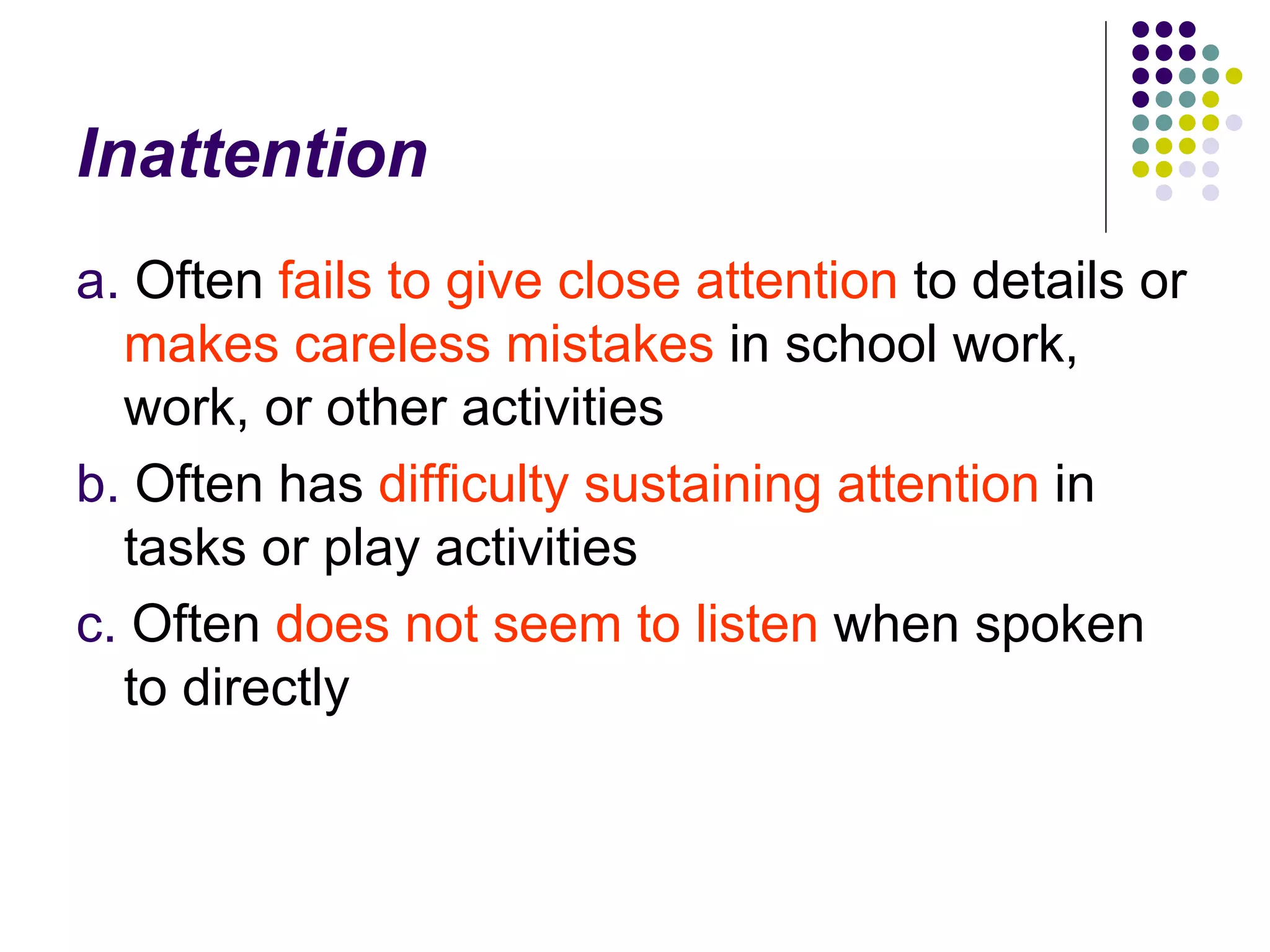
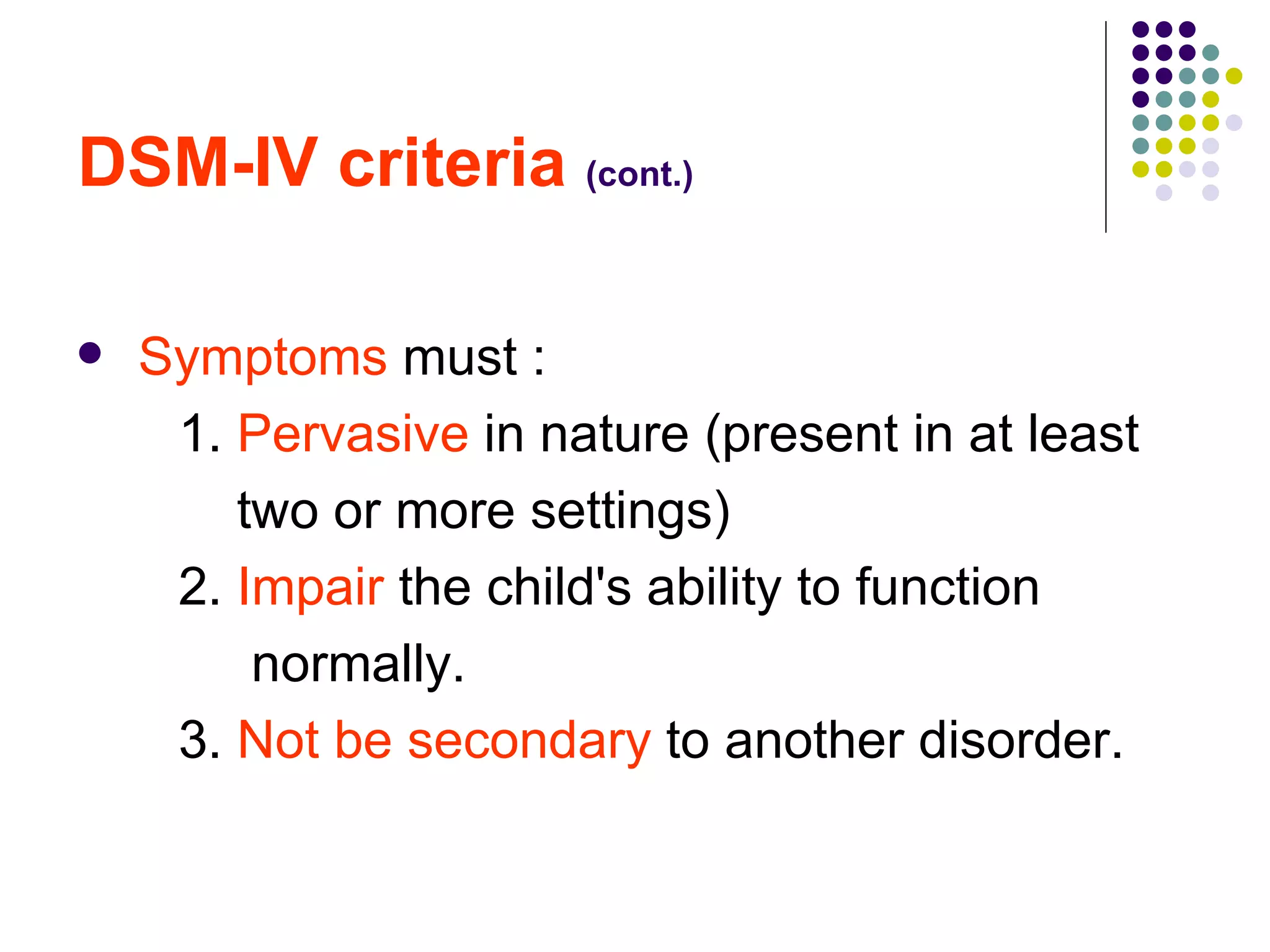
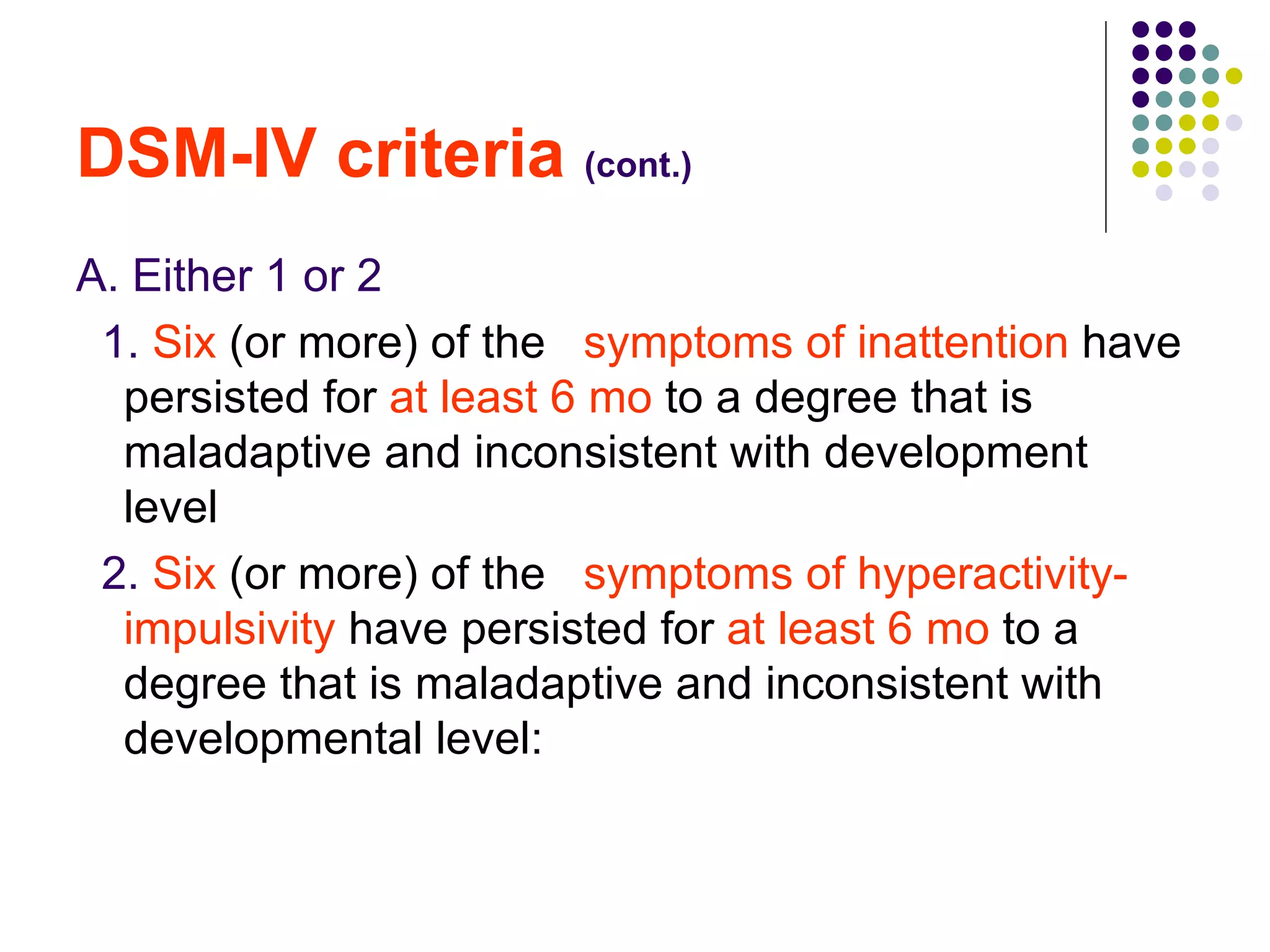
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurobehavioral disorders in children characterized by inattention, hyperactivity, and impulsivity. It is diagnosed based on symptoms that cause impairment in multiple settings according to the DSM-IV criteria. Treatment involves psychosocial interventions, behavior management training, and stimulant medication which effectively treat the core symptoms of ADHD.
![Attention-Deficit / Hyperactivity Disorder (ADHD) Prof. Saad S Al Ani Senior Pediatric consultant Head of pediatric Department Khorfakkan Hospital Sharjah ,UAE [email_address]](https://image.slidesharecdn.com/attention-deficit-100815065121-phpapp02/75/Attention-Deficit-Hyperactice-Disorder-1-2048.jpg)
![DSM-IV criteria (cont.) B. Some hyperactive-impulsive or inattentive symptoms that caused impairment were present before 7 yr of age . C. Some impairment from the symptoms is present in 2 or more settings (e.g., at school [or work] or at home).](https://image.slidesharecdn.com/attention-deficit-100815065121-phpapp02/75/Attention-Deficit-Hyperactice-Disorder-18-2048.jpg)