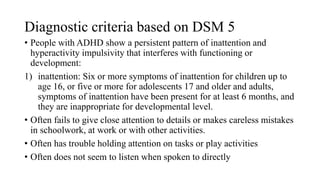
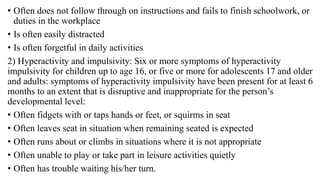
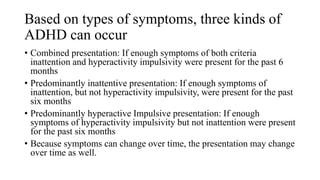
Attention Deficit Hyperactivity Disorder (ADHD) is characterized by patterns of inattention, hyperactivity, and impulsivity, affecting 3-5% of school-age children, with a higher prevalence in boys. ADHD has three subtypes: predominantly inattentive, predominantly hyperactive-impulsive, and combined presentation, and can lead to challenges in social and academic functioning. Treatment typically involves a combination of pharmacotherapy, psychotherapy, and behavioral interventions to address symptoms and improve overall functioning.