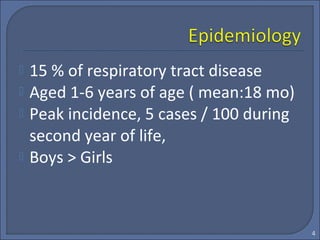
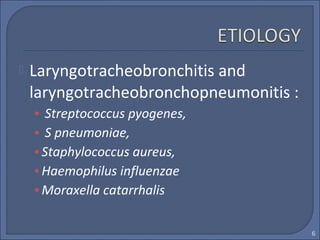
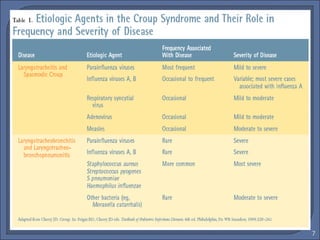
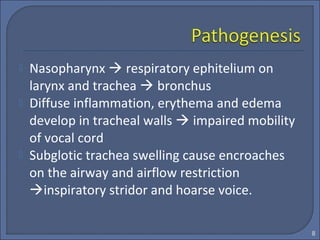
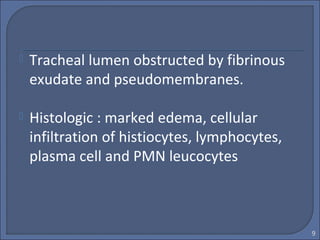
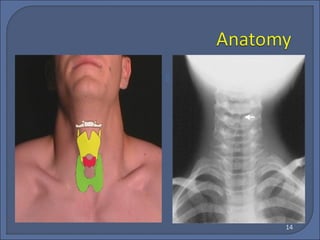
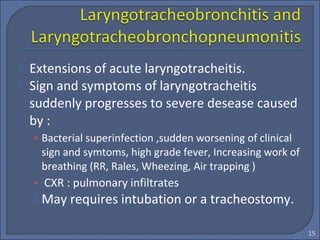
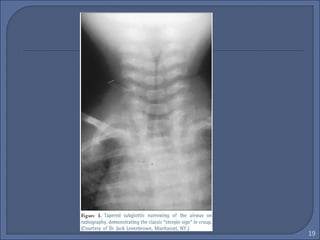
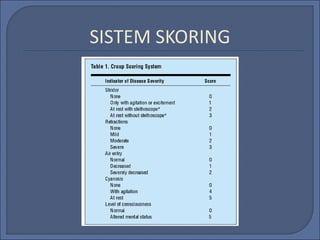
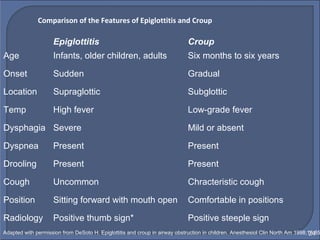
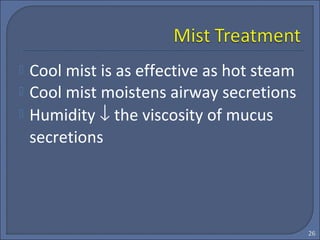
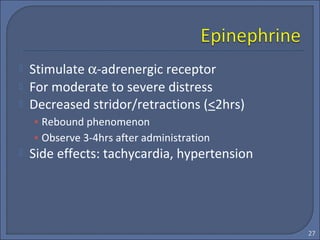
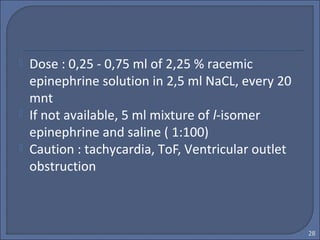
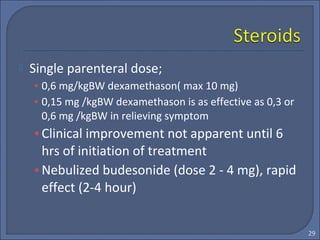
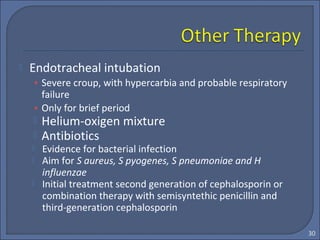
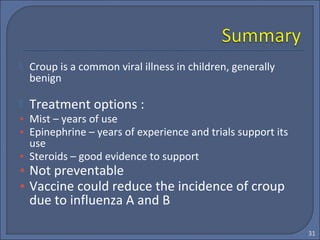
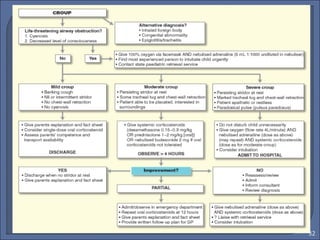
This document discusses croup syndrome, which refers to a group of respiratory diseases affecting the larynx, trachea, and bronchi. It manifests as hoarse voice, barking cough, inspiratory stridor, and respiratory distress. The most common cause is acute viral laryngotracheitis from parainfluenza viruses. Treatment involves mist therapy, epinephrine to relieve symptoms, and steroids to decrease inflammation. Croup is generally self-limiting and mainly treated with supportive care.