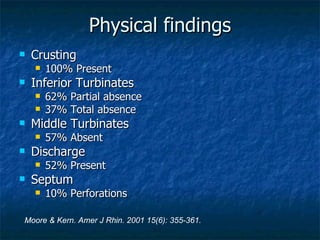
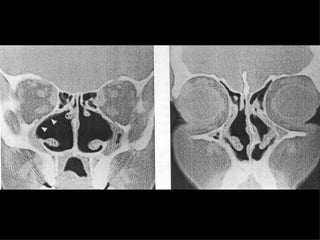
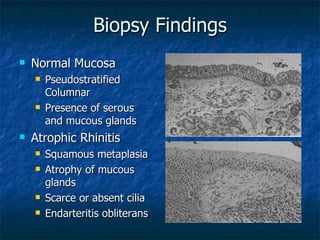
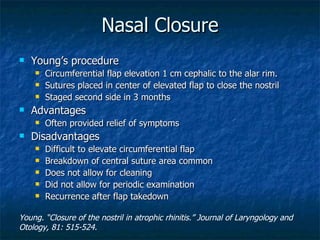
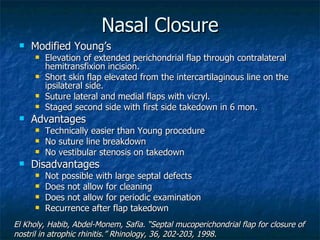
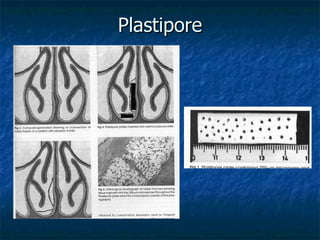
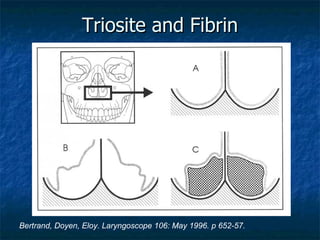
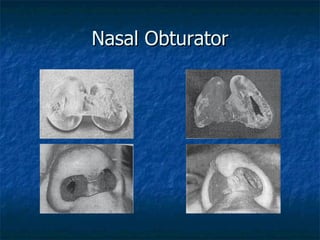
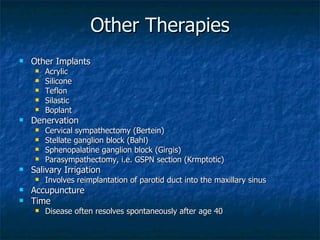
Atrophic rhinitis is a chronic inflammatory disease characterized by crusting, fetor, and atrophy of the nasal structures. It is most commonly caused by complications from prior sinus surgery. On physical exam, patients typically have extensive nasal crusting and anosmia. Radiographic findings include mucosal thickening and bone resorption in the paranasal sinuses. Treatment options aim to restore nasal hydration and minimize crusting, using topical therapies like saline irrigations and systemic antibiotics. Surgical therapies include closure of the nostrils or implantation of materials to increase nasal volume.