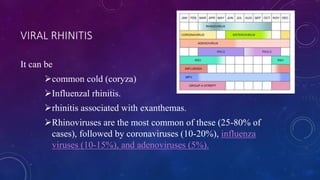
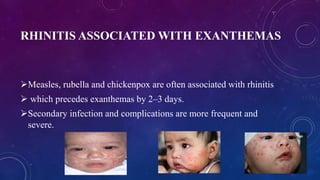
1. Acute rhinitis can be caused by viruses, bacteria, or irritants and causes symptoms like nasal congestion and discharge. Common cold is the most frequent type of viral rhinitis.
2. Chronic rhinitis can develop from recurrent acute rhinitis and causes long-term nasal obstruction and discharge. Types include chronic simple, hypertrophic, and atrophic rhinitis.
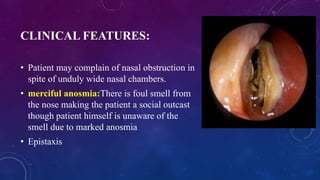
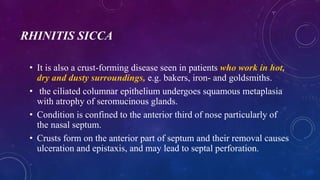
3. Atrophic rhinitis (ozaena) involves loss of nasal tissue and foul smelling crusts. It is usually treated through regular nasal irrigation, local antibiotics, and surgery to narrow the nasal cavity.